Imagine doing all the right things for patient care and forgetting a simple deadline and losing Medicare payments. The Merit-based Incentive Payment System (MIPS) has a lot of significant dates each year.
If you participate in MIPS for 2025, here’s the timeline you need to be aware of. Forgetting a deadline might result in penalties or lost incentives.
In this article, we will break down the MIPS 2025 reporting timeline in simple language. We’ll tell you what MIPS is, why it’s significant, and provide you with a simple list of MIPS deadlines for 2025. We’ll also provide plain tips to remain on track and meet CMS MIPS regulations.
Let’s keep MIPS as simple as possible!
What is MIPS and Why Should You Care?
MIPS stands for a Merit-based Incentive Payment System. MIPS is a Centers for Medicare & Medicaid Services (CMS) program that affects how Medicare pays physicians. You can consider MIPS a report card for physicians and medical professionals.
You get a score annually based on four performance categories:
- Quality – The degree to which you provide care (measured by some health outcomes and best practices).
- Cost – How well you care for people (CMS estimates this from your Medicare claims).
- Improvement Activities – What other things you do to enhance care (e.g., to help coordinate care or activities to educate patients).
- Promoting Interoperability – How effectively you utilize electronic health records and technology to enhance patient care.
Your MIPS score (0 to 100 points) is converted into an adjustment on your subsequent Medicare payments. Briefly:
- Do well (high score) – Possible bonus on your Medicare payments in a future year.
- Do poorly (low score) – Penalty (payment cut) on your Medicare payments in a future year.
- Score near the performance level of Neutral (neither penalty nor bonus).
For the 2025 performance year, the performance threshold is 75 points (this is the minimum score to not get a penalty per CMS for 2025).
That’s why MIPS is important. It can impact your money. It’s actual money at stake. Each point counts, and each deadline in the MIPS process is an opportunity to secure your points.
To comply with MIPS guidelines, you must provide the right data at the right moment. The guidelines and deadlines may be confusing, but we will simplify them.
Below is a straightforward timeline for MIPS 2025. We will start in late 2024 (preparing for 2025), provide critical dates in 2025, and move on to 2026 when you provide your data and get your results. Don’t forget to put these dates on your calendar!
Late 2024: Ready for the 2025 MIPS Year
The MIPS 2025 performance year officially begins with work at the end of 2024. Below are the main steps prior to 2025 starting:
October 1, 2024:
Virtual Group Election Begins: If you’d like to join or form a Virtual Group for MIPS 2025, the election window begins on October 1, 2024.
A virtual group lets solo practitioners or small practices groups online and report MIPS as a group. This might be handy if you’re a small practice and would prefer to share resources with others.
Why it’s important: Forming a virtual group may be able to boost your MIPS score by pooling performance data.
What to do: If you’re interested, speak to other clinicians in due course and have the formal arrangement written up. You have until the end of the year to do this (below).
November 2024:
CMS Final Rule Published: Early in November, CMS releases the Medicare Physician Fee Schedule (PFS) Final Rule for Calendar Year 2025.
This rule contains all of the official MIPS policies for 2025. For example, the final rule settled on the fact that the MIPS performance threshold remains 75 points in 2025.
Why it matters: The final rule informs you exactly what the MIPS requirements are in 2025 – what measures are available, how scoring is done, and if there are program changes or not.
What to do: Keep an eye on the final rule announcements from CMS. You don’t need to read the whole rule (it’s long!) but look for summaries applicable to MIPS. We will highlight any significant changes that impact on your reporting.
December 2024:
Check Your Initial MIPS Eligibility: CMS determines annually who must participate in MIPS. The initial MIPS eligibility information for 2025 will be available in December 2024.
CMS considers your practice’s Medicare billing and type of provider earlier in the year to determine whether you can participate in MIPS for 2025.
Why it matters: Not all clinicians must complete MIPS. If you are new to Medicare or have few Medicare patients or billing, you may not need to participate. Knowing your status is important.
What to do: Utilize the CMS QPP Participation Status Tool (on the QPP website) to review your MIPS eligibility for 2025 when available in December. Simply put in your NPI to determine if you must report.
If you discover you are not eligible, you will not need to report MIPS (but you may elect to report voluntarily). If you are eligible, then continue to follow the timeline below.
Dec 31, 2024:
The 11:59 p.m. ET Dec 31 deadline to file a virtual group election with CMS for the 2025 performance year.
Why it matters: You can’t form a virtual group for 2025 after this time.
What to do: If you wish to be in a virtual group, ensure you send your election to CMS by midnight Eastern Time on New Year’s Eve. It is wise not to leave it until the last minute in case of technical issues. CMS will then approve the virtual group if all qualifications are fulfilled. Then you and your group members will report MIPS collectively in 2025.
When next year arrives, you will know whether you qualify and whether you are reporting MIPS alone, in a group practice, or in a virtual group. You will also have CMS’s final 2025 rules. Now we can consider the 2025 performance year.
2025: Key Dates for MIPS Performance
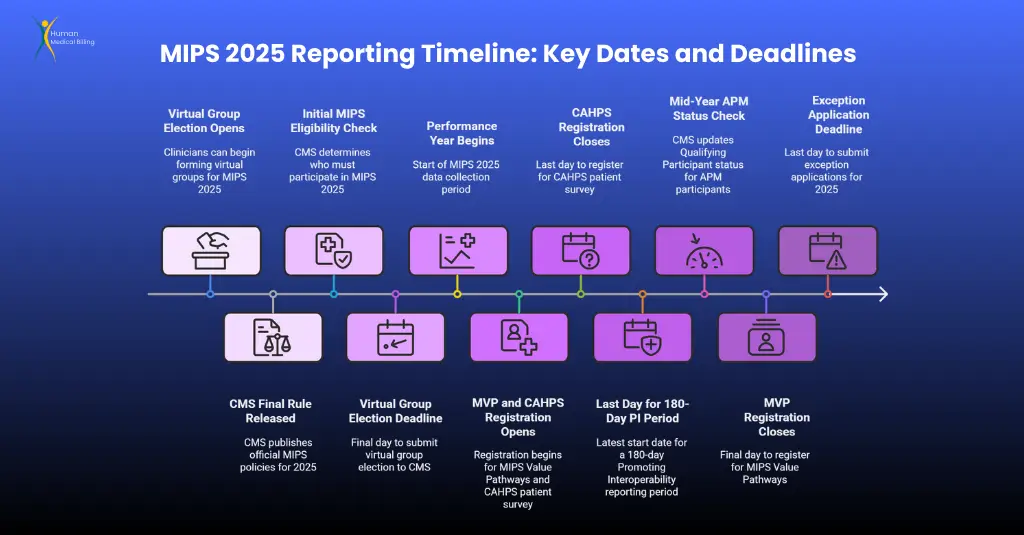
From January 1, 2025, to December 31, 2025, is the 2025 MIPS performance year, which is crucial for data collection. Human Medical Billing assists providers in meeting deadlines so they can comply with the rules and enhance MIPS scores. The critical dates are:
Jan 1, 2025 – Performance Year Starts: Start collecting data for MIPS domains (Quality, Improvement Activities, Interoperability). Audit quality metrics, start Improvement Activities for no less than 90 days, and have EHR in place. You can begin entering early 2025 MIPS data to track progress.
April 1, 2025 – Registration Begins:
- MIPS Value Pathways (MVPs): Enroll in individual MVP reports by December 1, 2025 (8 p.m. ET).
- CAHPS for MIPS Survey: Register by June 30, 2025 (8 p.m. ET). if you are employing this patient experience survey. Organizations utilizing CAHPS in an MVP must register for both.
- Spring/Summer 2025 – Exception Application Window Opens: You can apply for Extreme and Uncontrollable Circumstances (EUC) or Promoting Interoperability (PI) Hardship Exceptions up to December 31, 2025 (8 p.m. ET). Human Medical Billing suggests applying early for such issues as disasters or EHR issues to redistribute the burden of affected categories.
- June 30, 2025 – CAHPS Registration Closes: CAHPS enrollment deadline (8 p.m. ET). Complete MVP registration, if necessary.
- July 5, 2025 – 180-Day PI Reporting Deadline: Begin a 180-day Promoting Interoperability period by this date to report data for six months. Be aware of October 3 for at least 90 days.
- July 2025 – Mid-Year APM Status Check: Verify QPP Participation Status Tool for Qualifying Participant (QP) status using the March 31, 2025 APM snapshot. QPs are exempt from MIPS; others continue reporting.
- October 3, 2025 – Last Day for 90-Day IA/PI Reporting: Initiate 90-day periods for Improvement Activities and Promoting Interoperability. Record activities using the assistance of Human Medical Billing to remain compliant.
- October 2025 – APM Status Update: Check June 30, 2025 APM snapshot with QPP tool. QPs do not report MIPS; others continue and report.
- December 1, 2025 – MVP Registration Deadline: Register for MVP by 8 p.m. ET.
- December 2025 – Final MIPS Eligibility: CMS verifies eligibility based on data as of August 31, 2025.
- December 31, 2025 – Close of Performance Year: Complete data collection and submit exception requests by 8 p.m. ET.
Human Medical Billing helps you complete all quality measures and surveys, get ready to report your 2025 MIPS data to CMS and to receive their payment adjustments and feedback. Get back on track and improve your score with our help.
Early 2026: Your 2025 MIPS Data Submission
The submission time for the 2025 MIPS performance year is in early 2026.
The key dates are:
1. January 2, 2026 – Submission Window Opens: The submission window for 2025 MIPS data opens at qpp.cms.gov. You can begin uploading or validating your information through the QPP portal, a registry, QCDR, or EHR.
Human Medical Billing simplifies this and ensures Quality, Improvement Activities, and Promoting Interoperability (Cost is determined by CMS) data to be accurate. Begin early so you can fix mistakes since you can resubmit within this period.
2. March 31, 2026 – Submission Window Closes: Report 2025 MIPS data by 8 p.m. ET at qpp.cms.gov. Not reporting will earn a 0 score and 2027 penalty, with exceptions only if CMS states otherwise.
We recommends reporting early in March in the event of technical issues. Check for receipt on the QPP portal and monitor initial scores after submission.
Tip: Get in early (try mid-March) so you don’t stress and encounter technical problems. Remember the 8 p.m. ET deadline (5 p.m. PT) if you are not on the East Coast.
Mid 2026: MIPS Final Scores and Payment Adjustments
Payments based on the 2027 MIPS score will be finalized in 2026 through the 2025 submission cycle.
In mid-2026: Early Summer 2026 – Final Score Distribution Date: QPP posting of 2025 MIPS pre-validated final scores, which is expected by June 2026.
Ensure all ratios reflect your Performance Feedback Report. Your score determines the change in payment adjustment (positive, negative, or neutral) to Medicare payment for 2027. If discrepancies are detected, file a review request.
Initiation of Targeted Review Phase: Initiate the targeted review phase via QPP portal, one week after score release, for participants where score calculation appears erroneous (data was not accounted for, etc.). Resolution evidence should be submitted without delay.
Pay Changes Pre-Effective Date Summer 2026: CMS in July makes a public announcement for payment changes defining the alteration amount applicable from payment year 2027.
Determine the extent of payment increase or decrease for an individual, e.g. total (up to 0%) or (down 9%). Through feedback report estimate individual change, e.g, 1% or 3% increase of payment estimate for the income stream from Medicare.
Late Summer 2026 – Deadline to Request a Review: The review will occur around 30 days from the time the payment adjustment data become available (around late August 2026). Please request it prior to this deadline since requests for appeals cannot be requested once this deadline is reached. See the QPP portal for the review outcome, which is final.
They will determine your final score and your Medicare payment adjustment for 2027 by the summer of 2026.
January 2027: Payments under MIPS start to shift.
January 1, 2027:
Payment Adjustments Start: Payment adjustments for the 2025 MIPS performance year go into effect on January 1, 2027.
Starting with services you render in 2027, your Medicare payments will be adjusted up or down depending on your 2025 MIPS score.
Why it matters: This is the whole point of MIPS – the reward or penalty period. It runs for the entire calendar year of 2027 (January 1 to December 31, 2027).
What to do: When you start receiving Medicare payments in 2027, check your remittance advice or Medicare payment notices.
You should notice the adjustment applied. For example, if you got a +1.5% MIPS bonus, you’ll see payments are slightly higher (Medicare will apply that factor).
If you got a -4% penalty, your payments will be reduced by 4%. Ensure your billing department knows about these adjustments. There’s nothing to do actively at this point other than be aware.
Also, use this as feedback: if you got a penalty, consider how to do better next time; if you got a bonus, congratulations – try to keep the momentum going! And remember, 2027 adjustments are based on 2025 performance, so by this time you would have already done (or be doing) your 2026 MIPS reporting.
A reminder for the future regarding changes: CMS can alter MIPS rules or deadlines, so watch for any announcements. The following timeline is according to the official CMS 2025 MIPS year calendar.
If CMS ever alters a deadline or policy (for instance, they have sometimes moved up submission deadlines for special events), we will update this timeline. Always double-check that you are viewing the most current information, particularly as deadlines approach.
Considerations for Staying Within the Scope of MIPS in 2025
Towards successfully managing MIPS in 2025 and beyond, take note of these suggestions provided by Human Medical Billing Deals with MIPS:
1. Make a Schedule with Important Milestones: Put on your calendar the 2025 MIPS milestones, for example CAHPS Registration on June 30, 2025 and Submission of Data on March 31, 2026. Human Medical Billing will be there for each of those dates. Act on them promptly.
2. Develop Your Own Work Plan: Creating 2025 MIPS checklists with benchmarks and milestones such as checking eligibility as of December 2024 and submitting as of March 2026 is highly encouraged.
3. Assign Tasks Based on Specific Work: Split up tasks, for example Delegate Quality measures, Improvement Activities, and parts of EHR work to other staff members and follow up monthly. Solo practitioners should hire Human Medical Billing.
4. Track These Dates: Make use of the reporting and tracking capabilities available through registries.
Organize all documents accurate with headings such EHR snapshots, quality measures spreadsheets, and related documents to their appropriate folders. Human Medical Billing will check and organize these documents for these audits clients will require.
Conclusion
MIPS does not have to be intimidating. With this MIPS 2025 reporting schedule, you can know what to anticipate for the entire performance year and beyond. We started with planning measures in 2024, worked through each quarter of 2025 highlighting major deadlines, and carried on the process on through 2026 when you report and review your results, through to the payment changes in 2027. The process is lengthy, but every step is simple if you prepare for it.
The aim of MIPS is to improve patient care and reward physicians for quality work and improvement. By tracking MIPS deadlines for 2025, you will avoid penalties and also position your practice for potential bonuses while demonstrating that you are committed to quality care.
We hope that this breakdown made sense (as we said we’d do, explaining it like to a middle-schooler!). Have this guide handy throughout the year. If you ever ask yourself what comes next, consult the section for that time. We’ll follow up on this post if CMS publishes any updates, so you’ll always have the most up-to-date information.
Keep this guide handy and consult Human Medical Billing for updates or assistance. Plan ahead and you will succeed in MIPS 2025!


















