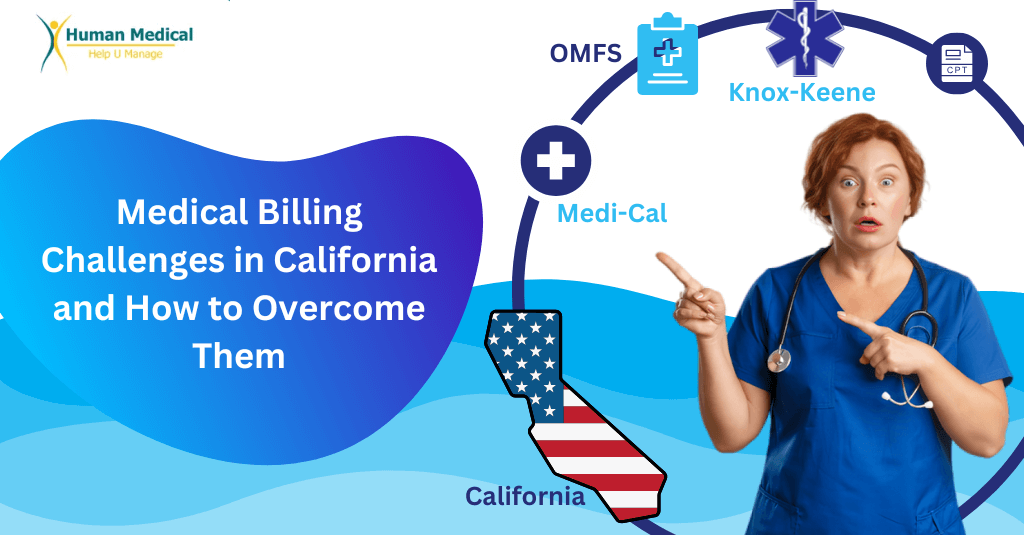
California’s healthcare is diverse and dynamic. For healthcare providers, making sure the billing is done accurately and paid on time in this state can seem remarkably complicated.
The state has strict rules and many diverse insurance companies, hence why medical billing in California is challenging and complex. These are not only in the domain of financial viability or stability but rather adherence, productivity, and, fundamentally, patient care.
Let’s look deeper into these unique Medical Billing Challenges and some strategies to address them.
Understanding the Fundamentals of Medical Billing
Medical billing is one of the management aspects of health care. It translates services offered into standardized codes that insurance companies understand. These include CPT, ICD-10, and HCPCS. They ensure that payments are accurate.
California complicates matters with specific rules, including Medi-Cal requirements and the Official Medical Fee Schedule (OMFS) for workers’ compensation cases.
Following these special standards is very important to prevent denials and penalties. Exact medical coding is a must to reduce claim mistakes to ensure billing correctness. Providers can benefit from services like medical coding services to fulfil payer needs and make workflows easier.
Unique Medical Billing Challenges in California
1. Dealing with Complex Insurance Payers:
California’s diverse population automatically means that healthcare providers need the skills to navigate an entire spectrum of insurance providers, from private to governmental programs and Medi-Cal.
Every payer has different rates, documentation requirements, and coding guidelines, making the billing process difficult. Such challenges in Medical Billing require deep expertise and meticulous management.
Partner with experts in Healthcare Revenue Cycle Management for a seamless management process in this regard.
2. Navigating Regulatory Compliance:
Providers must follow strict rules set by California laws, like the Knox-Keene Act and HIPAA. Medi-Cal has its own specific coding and paperwork standards, and there are special rules for workers compensation cases that need careful attention.
Not following these rules can lead to denied claims, fines, or even losing the ability to operate. Using services like medical billing services helps ensure compliance and lowers the chance of mistakes.
3. High Denial Rates:
The claims in California are often denied more frequently because of strict payer rules and laws that are complicated. Some usual reasons for denial include missing documents, wrong codes, and non-compliance with payer-specific rules.
When the claims are denied, it slows cash flow and takes more work to get the issues rectified. The providers can effectively handle these problems by using denial management services.
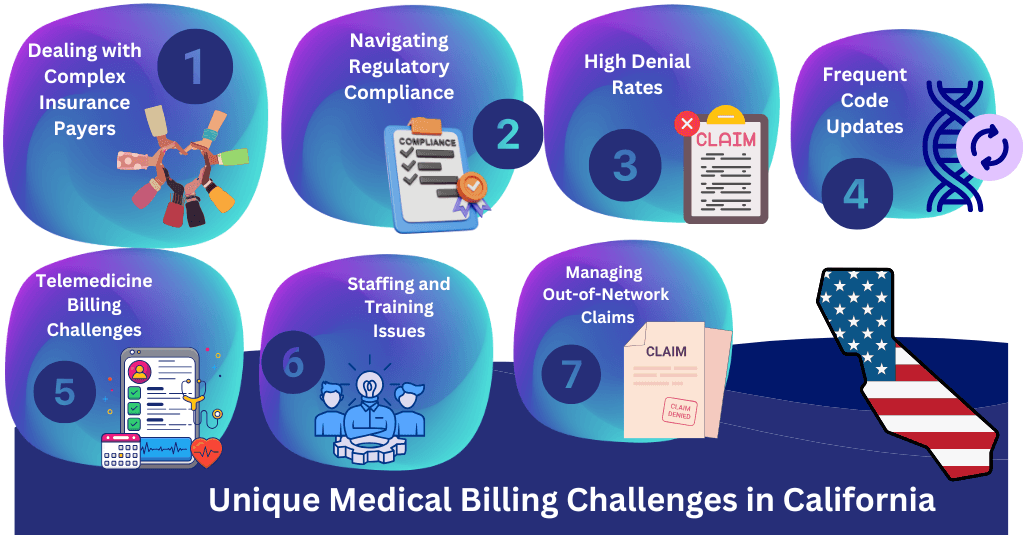
4. Frequent Code Updates:
The health care system of California is always changing, and billing codes and rules often change. Therefore, it is essential to update to ensure billing is correct and avoid claim rejections. Providers can benefit from working with experts who understand medical credentialing services and the latest rules.
5. Telemedicine Billing Challenges:
Billing is becoming more complex due to the growth of telemedicine. Online visits and remote monitoring require different paperwork and coding rules, which are payer-dependent.
Solutions to these specific medical billing challenges help in getting paid for telehealth services. Providers can make telehealth payments easier by using advanced tools and hiring experts.
6. Staffing and Training Issues:
It is difficult to source and retain competent billing personnel familiar with California’s special rules. Repeated training costs money. Recruiting specialists like Human Medical Billing will alleviate much of this issue.
7. Managing Out-of-Network Claims:
More to add to the difficulties of the process are California’s strict laws surrounding surprise billing and out-of-network reimbursements. Such issues tend to cause disagreements or delayed payments in revenue cycles. Such obstacles can be combated with integrated solutions such as denial and revenue management services.
Proven Ways to Solve Medical Billing Challenges
1. Pay Attention to Accuracy and Training
Training billing staff regularly is important in keeping up with California’s rules. Accurate documentation and coding from the beginning can help lower claim denials. For example, specialized medical coding services make sure everything is correct and follows the guidelines set by payers.
2. Use Advanced Technology
AI-powered billing eliminate errors, facilitate the claim submission process, and provide real-time denial tracking. Sophisticated solutions, such as AI medical billing, are required for dealing with constantly updated codes and the issues surrounding telemedicine billing. Such solutions adapt to the changes in rules and reduce the manual work burden.
3. Outsource to Experts
A medical billing company that understands the specific challenges in California will help reduce administrative work and enhance collection rates. Medical accounts receivable services will help providers to better manage cash flow and focus on patient care.
4. Improve Patient Communication
Clear billing practices help in building trust and reducing confusion. Clear explanation of co-pays, deductibles, and out-of-pocket costs will help the patients understand it better. Flexible payment plans and online portals make things easier for patients.
5.Regular Audits and Reviews
Routine audits pinpoint recurrent problems and increase the accuracy of information. Providers who audit bi-annually report a 20% increase in revenue cycle efficiency. Learn more about how our audits and review works.
6. Simplify Denial Management
A focused approach to denial management enables providers to recover revenue quickly. Reviewing denial trends and appealing denied claims in a timely manner ensures little disruption to cash flow. Learn how denial management services can transform your operations.
Future Trends in California Medical Billing
• Using AI
AI tools are taking over repetitive tasks, improving accuracy, and letting providers concentrate on patient care. AI medical billing services are creating better ways to handle billing.
• Value-Based Care
California is moving towards value-based care that focuses on patient results. Billing systems need to change to fit performance-based payment models, making value-centered practices even more important.
• Changes in Laws
The No Surprises Act demands better transparency in billing. Keeping a step ahead with such changes ensures adherence and patient satisfaction. Changes to billing systems for laws build trust and efficiency.
• Telemedicine Evolution
The billing system should adapt to telehealth’s distinct needs. Effective coding for virtual care ensures proper reimbursement, which is crucial, especially as telemedicine becomes California’s permanent piece of healthcare.
• Enhancements in Data Security
Investing in strong cybersecurity measures will ensure that the patient’s sensitive information is safe from cyber-attacks, hence staying compliant with the HIPAA and CCPA standards. Upgraded security measures also boost patient trust.
Why Choose Human Medical Billing?
Human Medical Billing specializes in California’s unique medical billing issues. With over 20 years of experience, we offer:
• Knowledge of California-specific rules, including Medi-Cal and OMFS.
• State-of-the-art technology to simplify billing and minimize errors.
• Personal account managers for individualized support.
• Seamless connectivity with more than 25 EHR systems to make work easier.
Let us help you solve the medical billing problems which slow down your growth and efficiency.
Frequently Asked Questions (FAQs)
What are the three key issues California medical billing is having difficulty with?
The biggest concerns for California medical billing are compliance with state regulations, high denial rates, and other issues related to telemedicine billing.
How can providers minimize claim denials?
Providers can minimize claim denials through investment in proper documentation, training of staff from time to time, and utilization of more advanced denial management tools.
Is outsourcing medical billing worth it?
Yes, outsourcing to experts like Human Medical Billing improves compliance and streamlines workflows and enhances revenue collection.
What makes California's billing regulations unique?
California’s billing rules, like Medi-Cal and OMFS standards, are complex and require special know-how to tackle.