Medical Billing Services
Denial Management Services
Maximize Your Revenue Recovery
Denial claims can cost providers as much as 10% of their revenues, but Human Medical Billing brings lost revenue back on board and prevents future denials. Our denial management services help streamline your revenue cycle with AI automation and analytics, revealing root causes and assisting in appealing denied claims for faster reimbursements. These totally standardized denial management solutions maximize revenue potential. tailored to each patient's unique needs.
Denial Prevention Starts Here!

Why Choose Human Medical Billing For Denial Prevention?
We at Human Medical Billing have perfected denial management services as an art through years of practice and experience. Here is why:
Prevent Future Denials
Fast Denial Resolution
Insightful Reporting
Join the growing community of providers reducing claim denials
and maximizing reimbursements with Human Medical Billing's Denial Management Services.
Types of Denials We Handle in Our Denial Management Company
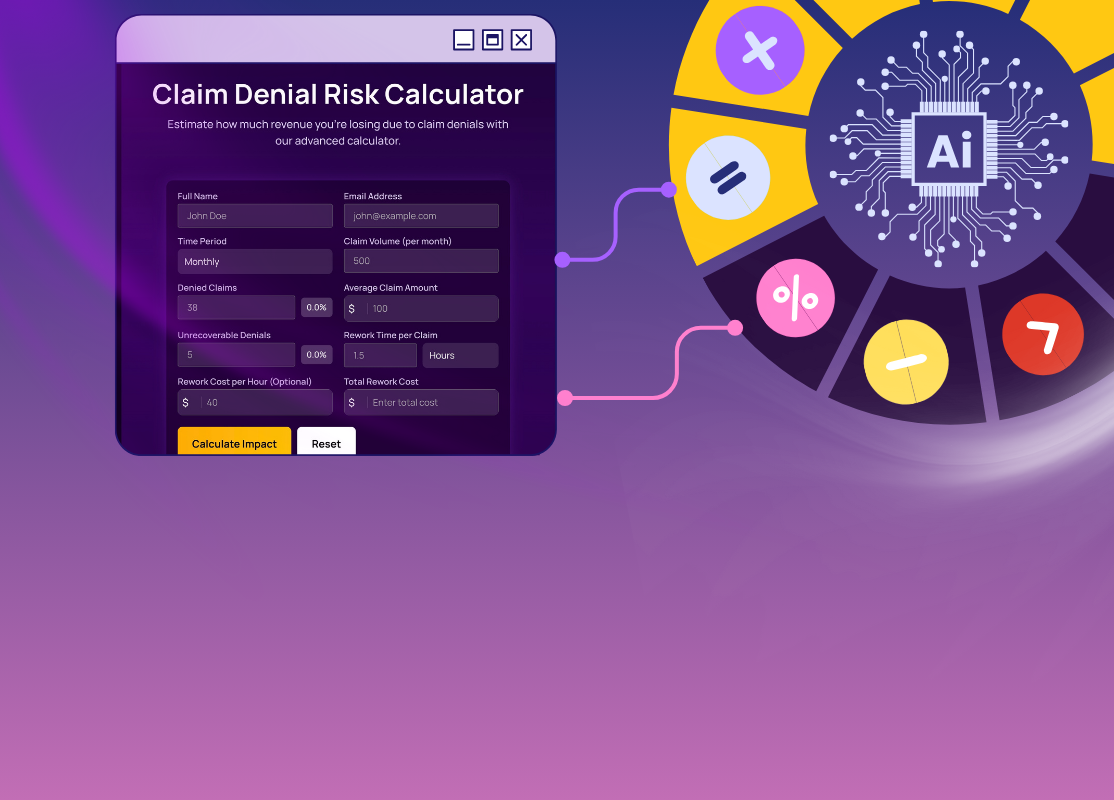
Denial Risk Calculator: Predict Claim Denials Instantly!
Calculate Your Risk for FREE!Administrative Denials:
Mostly due to coding errors, failure to qualify, and incomplete information submitted. Our team re-examines each of the denied claims and corrects the errors before resubmitting for payment.
Clinical Denials:
Sometimes, clinical denials are challenging due to medical necessity or lack of relevant documentation. Our specialists can construct extremely strong appeals for reconsideration of the claims.
Technical Rejections:
Applications are rejected due to format problems or inappropriate submission methods and therefore corrected and submitted promptly so that payment occurs more speedily.
Denial to Dollar: Convert Claim Rejections into Revenue
PATTERNS
ACTIONS
SUPPORT
Analyzing Denial Patterns
The services scrutinize patterns in claim rejections. They seek to find the common reasons behind them.
Implementing Corrective Actions
Based on analysis, these services take corrective actions. The goal is to reduce future claim rejections.
Streamlining Processes
They streamline your billing and coding processes. This reduces errors. Errors often lead to claim denials.
Appeal Support
Denial management services help prepare and file appeals for denied claims. This increases the chances of a successful overturn.
Staff Training
They train your staff on billing and claim submission. This prevents denials.
Technology Integration
They use advanced technology. Denial management services have automated systems. These make claims processing faster and reduce errors.
Continuous Monitoring
The services monitor claim status. They track the progress of appeals to ensure they are resolved on time.
Customized Solutions
Denial management services are tailored to your needs. They offer customized solutions to address unique challenges in claim denials.
What is Denial Management? How Human Medical Helps?
Denial management services involve identifying, analyzing, and resolving denied claims from insurance companies. At the Human Medical Billing Company, we specialize in proactive and effective denial management to help providers recover revenue that would otherwise be lost and implement strategies that prevent future denials, ensuring denied claims are reworked, appealed, and paid, making your practice financially stable.
Turning Rejections into Revenue
Our Denial Management Process
At the Human Medical Billing Company, we would have an efficient denial management strategy that would keep all claims handled and settled as soon as possible to recover revenue for you.
Tracking and Categorization of Denial
First, we track and classify denied claims based on the nature of denial, such as coding errors, eligibility, or incomplete documentation. AI automation helps track and classify claims faster, thereby making it more efficient.
Root Cause Analysis
Our team makes a deep analysis of denial and tries to understand why the claims are rejected. Either it would be a coding or documentation issue, but we learn the corrective measures not to go again for re-denial.
Rapid and Effective Denial Resolution
Our expert team will identify and correct coding errors, submit additional documentation, and challenge denials to ensure you receive your due reimbursements.
Appeal Preparation and Submission
In preparation for the claims being appealed, we prepare necessary documents and work with insurance companies to write smart appeals, evidence-based. So our team ensures that everything presented to them is likely approved.
Continuous Improvement
After denial resolution, we assess trends to potentially prevent any future issues as well. We offer resolutions in staff training, documentations improvements, and verifying patient eligibility to help maximize cash flow.
Claim Your FREE Practice Analysis!!
Frequently Asked Questions
What is Denial Management in Healthcare?
+Denial management in health care is related to the identification, analysis, and resolution of denied claims for the greatest revenue recovery. A structured denial management process helps the healthcare providers minimize loss, prevent future denials, and have an upward cash flow.
Why is Denial Management important for healthcare providers?
+Effective denial management is important as it affects the financial health of a provider right away. It not only assists in keeping steady revenues but also limits administrative burden since there are few repeating errors, while responses to denials are much faster.
How can denial management services improve revenue recovery?
+Denial management service looks at the cause of the denial then re-submits the claim in the right way so that it does not happen again. This approach allows the healthcare practice to recover their lost revenues and cash flows.
What are the most common reasons for claim denials in healthcare?
+The prime causes for denial are coding errors, missing documentation, eligibility issues, and authorization errors. Denial management services solve these issues by giving proper documentation, verification of the patient’s information, and proper accuracy in the coding done on the claim.
What steps are involved in the denial management process?
+Denial management, in general, involves tracking denied claims and root cause analysis followed by appropriate corrections and resubmittal of claims. Effective denial management requires training and process improvement throughout the processes to prevent such denials in the future.
How does technology improve denial management services?
+These include advanced technologies, such as AI and automation, that allow for better denial management through flags about possible errors, correction of claims by automating the process, and analysis of denial trends. These further result in quicker, more accurate resubmission and higher authorization approvals.
Can denial management services help with compliance in medical billing?
+Professional denial management services maintain compliance through proper submission of claims and adherence to coding and billing regulations on the part of healthcare providers. In other words, this reduces the probable risk of audits and penalties.
What are the benefits of outsourcing denial management?
+Health providers gain access to denied case expertise by outsourcing denial management, reduces administrative burdens, and enhances denial resolution. It therefore improves cash flow, increases fewer write-offs, and results in better patient care concentration.
How quickly can I expect results from denial management services?
+All the practices have shown huge improvement in terms of cash flow as well as fewer denied claims, particularly during the period of few months with experienced teams, by a structured approach.
Do denial management services work with all types of healthcare providers?
+Indeed, denial management services benefit most health providers, including hospitals, clinics, and specialty practices, from the aspect of overall financial health. The services may also be customized to fit the precise needs of each practice.
Get In Touch
- Send your comments through this form and we will get back to you. Or, For Enquiries Call:
- (877) 669 1070








