Medical billing is the process by which healthcare providers translate healthcare services into billing claims. These claims are then submitted to insurance companies to ensure providers are reimbursed for their services.
Medical billing is an essential ingredient for everyone in healthcare, whether you are a patient, a provider, or a member in administration.
Why Medical Billing Matters
Back in the States, healthcare providers need appropriate and timely medical billing for their businesses to stay in financial health. Hospitals, clinics, and private practices stay afloat with money from insurance companies and patient-paid claims.
When billing is not appropriate, providers may face delayed reimbursements, lost revenue, and even fines for rule violations. That is why trustworthy healthcare revenue cycle management services are a necessity today for practice.
The Essentials: What is Medical Billing?
Medical billing starts when a patient checks into a healthcare facility and continues until the provider is fully reimbursed. This involves translating everything that happens during the patient’s visit into a language insurance companies understand: a series of codes and detailed information.
The process needs to be accurate. Medical billing errors result in insurance carriers denying claims, holding up providers in receiving reimbursements, or even raising legal issues. Precision is not only recommended - it is essential for a successful revenue cycle and satisfied patients. Human Medical Billing gets each step carefully accomplished.
The Medical Billing Cycle Step by Step
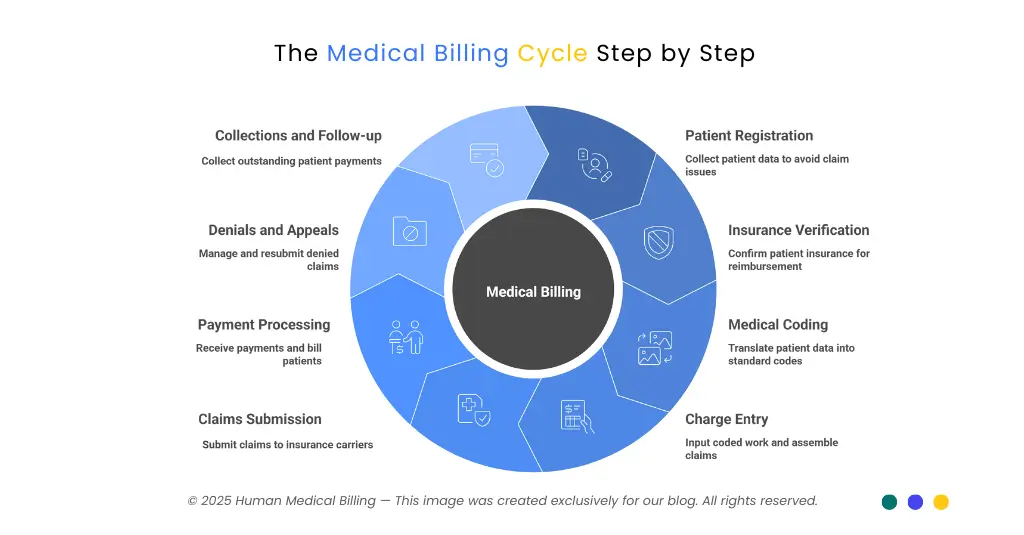
Let's break down the typical medical billing cycle used by most healthcare providers:
1. Patient Registration
This is the first and perhaps the most crucial step. Billers collect the patient's insurance information and personal information with a complete and accurate set of data. Proper registration reduces the likelihood of a denied claim due to missing or inaccurate information.
2. Insurance Verification
The second step is confirming if the patient is insured. This guarantees reimbursement for the services from this provider during this visit.
3. Medical Coding
They note a patient's symptom for a visit, diagnoses, and treatments. Medical coders translate this information into standard codes, e.g., ICD-10 for diagnosis codes and CPT for procedures.
(For expert help, think about our medical coding services.)
4. Charge Entry
Billers input all coded work assignments, input charge values, and assemble a claim.
5. Claims Submission
These claims are submitted (usually online) to insurance carriers. Most medical providers today utilize AI Medical Billing software for greater efficiency and accuracy in claims.
6. Payment Processing
If the claim is correct and complete, the insurance company pays the provider for the approved amounts. Patients then get bills for any charges not covered (like deductibles or copays).
7. Denials and Appeals
Now and then, claims are denied or paid less because codes are wrong, information is incomplete, or insurance coverage is flawed. Medical billers are supposed to recognize why it happened, fix it, and then resend the claim - this is called denial management services.
8. Collections and Follow-up
The final step is gathering any amount still due by a patient. specialized medical accounts receivable services prevent organizations from having unpaid bills and issues with their flow of funds.
| Step | Description |
|---|---|
| Patient Registration | Gather patient & insurance info |
| Insurance Verification | Check insurance coverage, eligibility |
| Medical Coding | Code diagnoses & procedures |
| Charge Entry | Enter charges and codes |
| Claims Submission | Submit claims to insurance |
| Payment Processing | Receive reimbursement, bill patient |
| Denials & Appeals | Fix errors and resubmit claims |
| Collections & Follow-Up | Retrieve remaining balances |
Key Terms in Medical Billing:
Having a minimum level of knowledge would allow everyone to manage medical billing:
- Claim: The bill sent to the insurance company.
- CPT Codes: These codes explain what procedures were performed.
- ICD-10 Codes: These represent the patient’s diagnoses.
- Co-pay: The portion of the bill the patient is responsible for during a visit.
Who Does Medical Billing?
Medical billers are individuals who usually possess certifications such as Certified Professional Biller (CPB) or Certified Medical Reimbursement Specialist (CMRS). These medical billers take care of everyday tasks and ensure each patient visit results in proper and successful claims.
These professionals stay updated on US healthcare regulations as well as payer requirements and continuously enhance their expertise in fresh technologies, including AI Medical Billing software. Human Medical Billing employs only professionals who are best in their field and up-to-date with everything.
Importance of Accurate Medical Billing
Correct medical billing is not only about receiving a check - it is also about complying with the rules. Federal laws such as HIPAA mandate stringent privacy and billing regulations.
Falsely sending bills, charging for treatments not administered, or failure to safeguard patient information may result in substantial fines and damage your credibility. Human Medical Billing's team is serious about those responsibilities.
Common Medical Billing Challenges
Medical billing is complicated, even better systems having problems like:
- Ongoing insurance policy and coverage changes
- Timely updates in medical codes and rules for compliance
- Delayed reimbursement for errors in claims
- We need secure technology to keep patient data safe.
Solutions: How to Succeed in Medical Billing:
To avoid known pitfalls, health workers rely on:
- Advanced Revenue Cycle Management for Healthcare
- Advanced AI Medical Billing software for claim verification and tracking
- Experience in Denial Management Services for denied claims
- Continuing training for employees with such sources as the Xpert Billing Blog
- Clear communication with patients about their financial responsibilities
Human Medical Billing implements all of these approaches. See our success stories and how our services work for actual examples of how we make our clients a success.
Technology Trend: The Rise of AI Medical Billing:
Healthcare is evolving rapidly. Using AI, intelligent systems review claims and identify errors before submission. Providers who utilize AI Medical Billing are paid sooner, make fewer errors, and comply better - all while minimizing stress on staff. This is a contemporary method of operation whereby staff is free more to focus on patient care rather than paperwork.
FAQ’s
It’s the process of creating, submitting, and following up on healthcare claims with insurers to receive payment for services.
Every healthcare provider, from small clinics to major hospitals, uses medical billing to get paid and keep their practice going.
Partnering with a specialist like Human Medical Billing, using up-to-date software, and providing continuous staff training are proven solutions.
It keeps healthcare systems running smoothly and helps patients avoid expensive billing mistakes.
Why Choose Human Medical Billing?:
Human Medical Billing is a medical billing company offering medical billing services with personalized solutions for any-sized practices. Whether denial management services or medical credentialing services or medical coding services. Accuracy is our prime focus along with compliance and patient satisfaction.
- Believe information supported by real results - refer to success stories.
- Transparency in Process - learn about us and how our services work
- Ongoing assistance - Contact us for a FREE analysis
Conclusion
Medical billing is an integral component of health care in America today. It ensures that every service is coded and processed correctly so providers are reimbursed for their service, patients are billed appropriately, and the system is strong and in compliance.
Medical billing is an ever-changing entity, but if you remain up-to-date, adopt new technologies, and make use of professionals like Human Medical Billing, providers are then able to concentrate on delivering great care rather than forms.