When claims are denied, many providers experience the frustration of waiting to receive reimbursement for the services they provided. They have submitted their paperwork and now just sit back and wait; instead of receiving the funds for the services rendered, they receive a letter stating the claim has been denied. Denial in medical billing is a subject many providers are familiar with as well as a problem they face each day. This brings us to a common question: What is denial in medical billing and how will it affect my practice?
A claim denial occurs at the time that an insurance company decides to deny payment for a medical service. A rejection is different; A rejection usually occurs prior to a claim being denied by the insurer. A rejection is generally caused by a format issue or typographical error preventing the computer system from processing the claim. A denial occurs after a claim has been reviewed by the insurer and they have determined not to make payment to the provider based upon the applicable policy language and requirements.
What is denial in medical billing?
Denial in medical billing is when an insurance company refuses to pay for a healthcare service that was submitted as a claim after it has been processed through their system. Unlike a simple rejection (which simply means they did not receive enough information to process the claim), a denied claim has been reviewed by an insurance representative, and found to be unable to be paid based on certain issues such as missing required documentation, lack of medical necessity, or that the claim was filed too late (Expired Filing Limits). Most denied claims can be either "Appealed or Corrected" so that the provider may recover some or all of the lost revenue.
Why Denials Happen
Insurance companies have many guidelines to follow. Even if an applicant leaves out just one item on their application, the insurance company will send it back to the applicant with no payment made. Below are some of the top causes of denials in medical billing:
- Missing Information: If there is a middle name left blank, a missing SSN (Social Security Number), or a missed field regarding your medical history, etc., then the payor will flag it and deny it.
- Duplicate Claims: In some cases, a provider sends a duplicate claim because they did it unintentionally. However, the system recognizes it as a duplicate claim and denies it.
- Lack of Medical Necessity: The insurance company may find that the service provided was not medically necessary for the patient's condition and therefore deny the claim.
- Prior Authorization: Some services require prior authorization before the provider provides the service. If the provider does not get the prior authorization from the payor first, then the claim will be denied.
- Expired Limits: All payors have a limited timeframe to file claims for payment. When the claim filing deadline is exceeded, the opportunity to receive payment for those claims is lost.
We see all of these trends at Human Medical Billing every single day. Our team helps providers recognize potential errors in their claims before they submit to the payor.
The Cost of Doing Nothing
It is costly when a medical provider does not address a denial in their medical billing process. Research indicates that the average cost to reprocess an individual denied claim is about $25. As a result, if your practice has hundreds of denied claims, the cumulative costs will be very high. Many medical practices do not resubmit denied claims which results in leaving thousands of dollars on the table each year.
A team of effective medical accounts receivable services can help prevent this from occurring by tracking all dollars for a patient from the time the patient is seen, through the entire claims process, and until final payment is received.
| Metric | Industry Average | Goal for High-Performing Practices |
|---|---|---|
| Denial Rate | 5% to 10% | Less than 4% |
| Clean Claim Rate | 75% to 85% | 95% or higher |
| Days in AR | 40 to 50 days | Under 30 days |
How to Manage Denials Effectively
You can’t simply respond to each denial as they come up. To be able to do so, you'll want to develop a plan. Denial management services are your best resource for this.
First, you need to determine how your denials are being caused. Are your denials occurring as a result of front office errors or coder error? For example, if the front office fails to verify coverage prior to submitting a claim, the claim will deny. Similarly, if the coder utilizes an outdated code when creating the claim, the claim will also deny.
Next, establish a time frame for appealing/correcting denied claims. In medical billing, you have approximately 48-72 hours from the date a claim is denied to file an appeal/attempt correction. The longer you allow to pass before filing an appeal/correction, the less likely you will receive payment on the denied claim.
Lastly, identify patterns/trends associated with denials. For instance, if a single insurance carrier consistently denies reimbursement for a particular CPT/ICD10 code, you may need to modify your internal processes regarding how you bill that specific payer.
The Role of Coding and Credentialing
The first step to achieving accuracy is by using the correct codes in medical billing. Medical coding services are used to ensure that all claims submitted contain the appropriate procedure(s) as well as the corresponding diagnosis for those claims. Therefore, medical coding services reduce the likelihood of a denial based on "medical necessity".
In addition, you should verify your provider's status with the insurance company. Each time a physician submits a claim for reimbursement, if he/she has not been properly enrolled with the particular insurance plan at hand, the claim will automatically be denied. A regular service such as medical credentialing services helps to maintain the eligibility of your physicians for reimbursement.
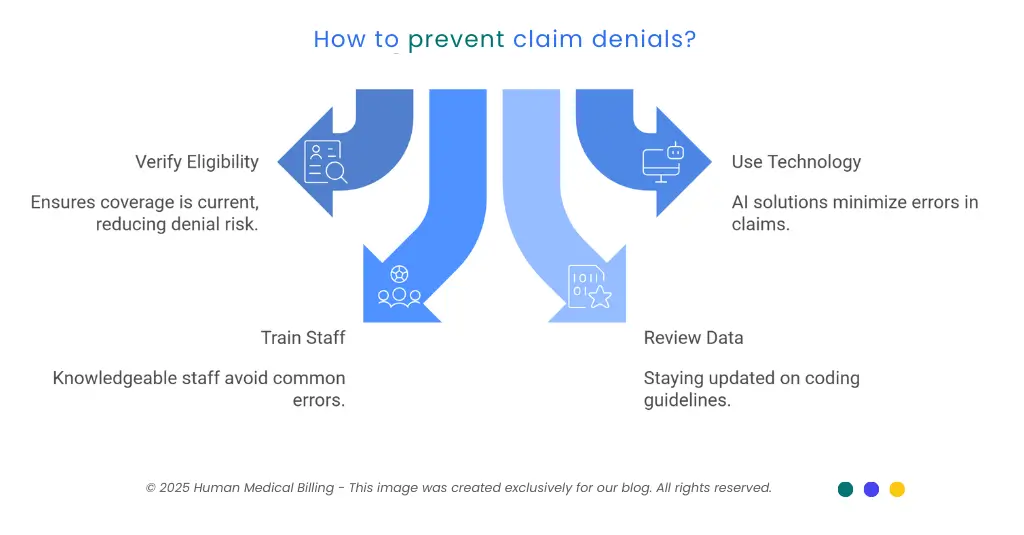
Preventing the Next Denial
It's always easier to prevent a denial of claim from happening in the first place. The same applies to your practice with medical billing.
The best ways to help avoid denial are as follows:
1. Verify Eligibility:
Verify the patient’s eligibility for coverage each time he/she visits. Insurance coverage can change often.
2. Use Better Technology:
Consider using modern AI based billing solutions that use AI to scan your claims prior to submitting them (the goal being to reduce errors).
3. Train Your Staff:
Train your staff to be knowledgeable about the most recent payer requirements such as those of Medicare and Blue Cross.
4. Review Your Data:
Review your data through the use of an Xpert billing blog or a similar resource to be aware of the most current coding guidelines.
To provide an example of this, the majority of errors occur at the front desk when the information is entered incorrectly by the person checking in the patient. When your front office staff accurately enters all of the necessary information at check-in, the rest of your medical billing service process will go much smoother.
The Human Side of Billing
While technology can be very useful, there are times when you need to speak directly with an insurance company to advocate on your behalf regarding your payment. Therefore, we refer to ourselves as "Human Medical Billing," by combining smart tools (technology) with real people with a strong understanding of the complexities of healthcare.
You will find in many of our success stories that these common problems exist in the same ways in many different practice settings. Many practices experience high denial rates and slow payments. By transitioning to professional healthcare revenue cycle management services, they are able to convert many of these denials into dollars of revenue.
Next Steps: Determine whether or not your current denial rate exceeds 5%. If so, you are losing money.
Frequently Asked Questions
Yes, most health insurance companies will let you file an appeal and, as part of this process, you need to send them documentation showing that the services provided were medically necessary and were submitted according to their procedures and guidelines.
Yes, a "soft" denial is considered temporary because, when you add a missing document(s) or correct the coding error, the denial becomes rescinded and you may resubmit your claim; on the other hand, a "hard" denial is considered final and typically indicates that the service(s) billed were not included under the terms of coverage of the patient's policy.
Medical billing AI uses algorithms to determine whether claims have been processed correctly so as to reduce the likelihood that those claims will be denied by the payer prior to submission; therefore, based on the information obtained from these algorithms, you can take corrective action on the claims to prevent a denial at the time of submission.
Work With the Experts
Managing a practice can be tough enough to worry about all the paperwork that comes with the insurance claims; that's why we've created our "About Us" section where you can read about what makes us unique; in short, we are about being transparent and providing real results.
Ready to improve your bottom line? Use our "Contact Us" page to get a complimentary analysis of your present billing process and find out what you are missing!
Final Thoughts
To get your medical billing on the right path, start by learning about denial and what it means for you in medical billing. Denial can be a source of improvement when you see them as data instead of simply a loss.
No matter if you need some support with your medical coding services or a complete revision of your denial management services; you are going to have less time spent on this area of your business when you act on this today.

