Having spent over a decade working in healthcare revenue cycle management, I can safely say that 2025 will be a turning point. We are faced with declining reimbursements, new technology, and regulatory updates that are changing the way we bill medically.
If you are feeling overwhelmed by the repeated stream of updates, do not worry, you are not alone. Let me walk you through what really matters for your practice this year.
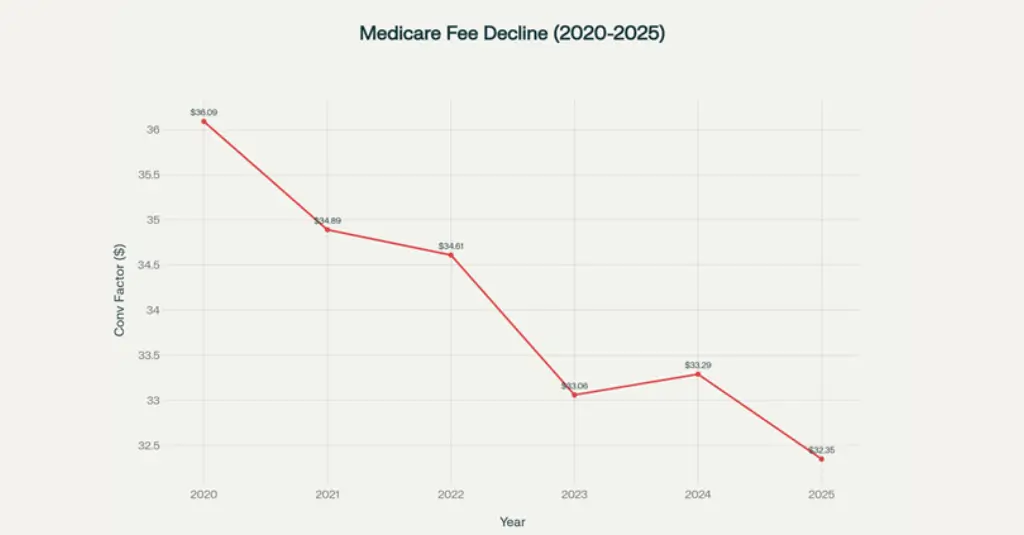
Medicare Physician Fee Schedule conversion factors have declined significantly from 2020 to 2025, with only temporary congressional intervention preventing steeper cuts.
The Harsh Reality of 2025 Fee Schedules
Let's start with the elephant in the room: Medicare reimbursements are getting squeezed hard. The 2025 conversion factor dropped to $32.35 - a 2.83% decrease from 2024's $33.29. When I see practices struggling to keep their doors open while providing quality care, this trend hits close to home.
What makes this particularly painful is the context. While your costs for staff, supplies, and technology keep climbing at 3.5% annually (per the Medicare Economic Index), your payments are moving in the opposite direction. It's like trying to run uphill while someone keeps making the incline steeper.
The Real Impact on Different Specialties
From my experience working with various practices, the impact isn't uniform across specialties. Radiology practices are getting hit especially hard, with some high-volume procedures seeing cuts beyond the baseline 2.83%. Breast tomosynthesis (G0279), for instance, saw a 9.67% reduction for 2025, following an 11.72% cut in 2024.
Primary care providers, on the other hand, might find some relief through the new Advanced Primary Care Management (APCM) codes, which bundle chronic care management services. It's CMS's way of acknowledging that preventive care should be valued differently than traditional fee-for-service transactions.
Navigating the 2025 CPT Code Revolution
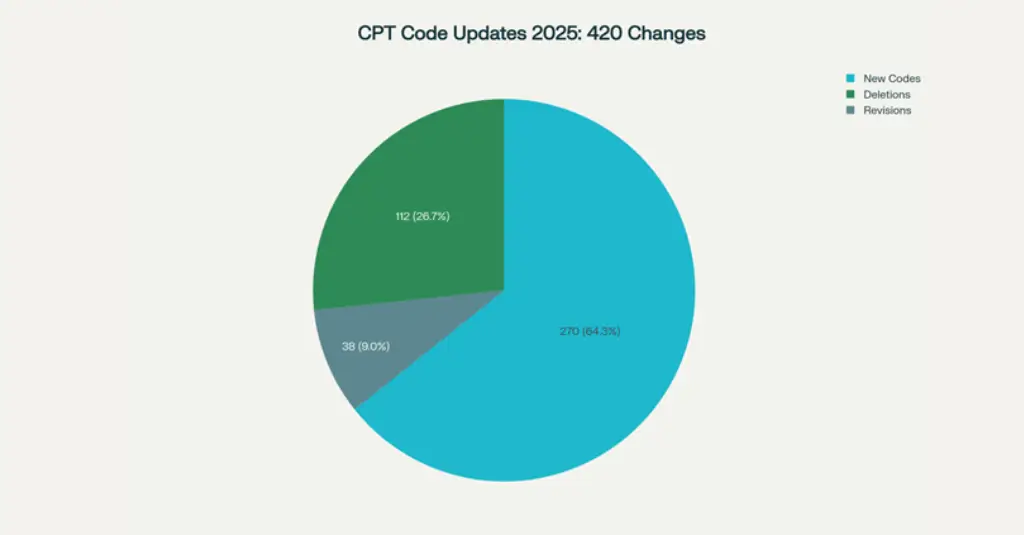
The American Medical Association introduced 420 CPT code changes for 2025, with nearly two-thirds being new codes reflecting advances in digital medicine and AI.
The 420 CPT code changes for 2025 represent one of the most significant updates we've seen. With 270 new codes, 112 deletions, and 38 revisions, your coding team needs to be ready for a substantial learning curve.
What's Driving These Changes
From my conversations with coding specialists, three areas are dominating the updates:
- Digital Medicine and AI Integration: The new AI taxonomy in Category III CPT codes is fascinating from a technological standpoint, but it's also creating billing complexity. These codes categorize AI services as assistive, augmentative, or autonomous distinctions that will matter for reimbursement.
- Telemedicine Expansion: The AMA introduced 17 new telemedicine codes (98000-98016) for synchronous audio-video encounters. However, here's the catch: Medicare has only adopted one of these codes (98016), and you'll still need to use traditional E/M codes with modifier 95 or 93 for most telehealth services.
- Remote Therapeutic Monitoring (RTM): New codes 98975, 98976-98978, and 98980 are expanding how we can bill for digital therapeutic interventions. This is where the industry is heading, and getting familiar with these codes now will pay dividends.
Implementation Strategy That Actually Works
Based on what I've seen work in real practices:
- Start with high-volume codes first: don't try to learn everything at once
- Create coding cheat sheets: for your most common scenarios
- Run parallel coding: for the first quarter, if possible, to catch mistakes
- Invest in claim scrubbing technology: to catch errors before submission
Prior Authorization: The Necessary Evil Getting More Complex
Prior authorization has become the bane of many practices' existence, and 2025 isn't making it easier. What I'm seeing across different payers is a trend toward more services requiring PA, coupled with tighter timelines.
The 10-Day Rule Changes Everything
Several major payers are implementing 10-day post-service review windows for medical necessity reviews. This means if you don't get your prior authorization submitted within 10 business days after providing the service, you're looking at potential denials.
Here's my practical advice for managing this:
- Automate Everything You Can: Electronic prior authorization systems aren't just nice to have anymore, they're essential. The practices I work with that have automated PA workflows are seeing 40-50% faster approval times.
- Create Service-Specific Checklists: Different specialties have different PA requirements. Cardiology practices need different workflows than dermatology clinics. Customize your approach rather than using one-size-fits-all solutions.
- Train Front-Office Staff: Your scheduling team needs to understand PA requirements as well as your billing team. Catching PA needs during scheduling saves massive headaches downstream.
No Surprises Act: What's Actually Working (And What Isn't)
The No Surprises Act has been in effect since 2022, and by most accounts, it's achieving its primary goal - over 25 million surprise bills have been prevented. But implementation hasn't been smooth, and there are still gaps that impact your revenue cycle.
Independent Dispute Resolution (IDR) Challenges
The IDR process, while functional, has some concerning trends. Median arbitration decisions are running at least 3.7 times what Medicare would pay for certain services. This suggests that out-of-network rates were potentially inflated before the NSA, but it also means the arbitration process might not be as balanced as intended.
From a practical standpoint, here's what you need to know:
- Good Faith Estimates Are Still Problematic: The requirement for uninsured patients is in effect, but Advanced Explanation of Benefits (AEOB) for insured patients is delayed pending further rulemaking. This creates a two-tiered system that's confusing for staff and patients.
- Documentation Is Critical: Every NSA-related case I've reviewed comes down to documentation quality. If you're not documenting patient consent for out-of-network services or maintaining proper good faith estimate records, you're setting yourself up for problems.
The RCM Playbook That's Actually Working in 2025
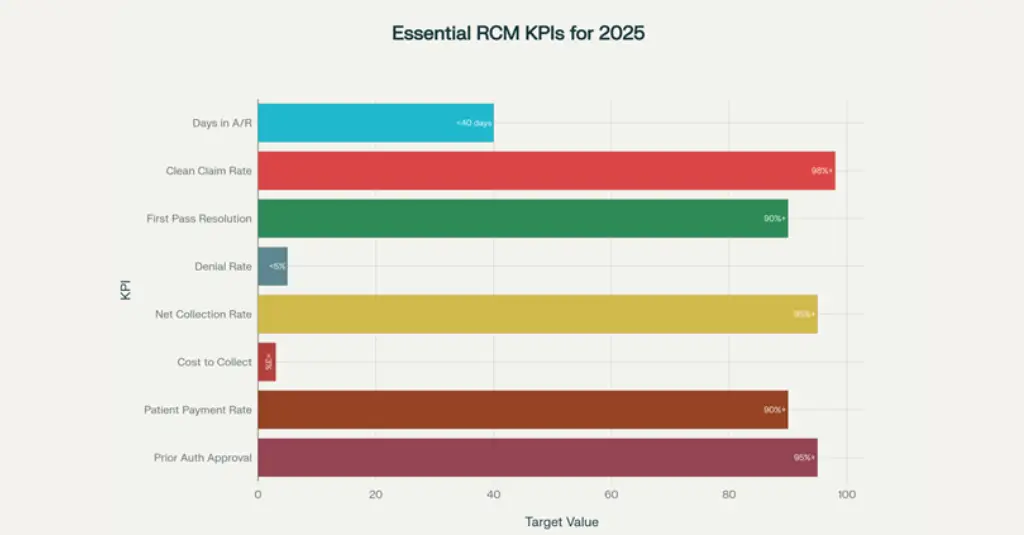
Key Performance Indicators (KPIs) every healthcare practice should monitor for optimal revenue cycle management in 2025.
Let me share what I've learned from working with practices that are thriving despite these challenges. It's not about having the most expensive technology, it's about getting the fundamentals right and using data to drive decisions.
The 8 KPIs That Matter Most
After analyzing hundreds of practices, these are the metrics that consistently predict financial success:
- 1. Days in Accounts Receivable (A/R): Keep it under 40 days. If you're above this, you have either collection problems or billing accuracy issues. The best practices I work with are hitting 30-35 days consistently.
- 2. Clean Claim Rate: Anything below 98% means you're losing money to avoidable rework. Investment in claim scrubbing technology pays for itself quickly when you hit this benchmark.
- 3. First-Pass Resolution Rate: Target 90%+. This metric tells you whether your initial submissions are accurate enough to get paid without back-and-forth.
- 4. Denial Rate: Keep it below 5%. Remember that 76% of denials are driven by missing, incomplete, or inaccurate data, most are preventable with better front-end processes.
- 5. Denial Management That Actually Prevents Problems: The practices seeing the best results aren't just managing denials, they're preventing them. Here's the approach that's working:
- 6. Front-End Prevention: Real-time eligibility verification and automated prior authorization tracking catch 80% of potential denial causes before claims are submitted.
- 7. Root Cause Analysis: Use data analytics to identify patterns. If you're seeing denials for specific CPT codes or particular payers, dig deeper. Often there's a systemic issue that can be fixed.
- 8. AI-Powered Claim Scrubbing: The technology has matured enough that AI can catch coding errors, missing modifiers, and documentation gaps before submission. The ROI on these tools is typically 3-4 months.
The AI Revolution in Medical Coding
AI is transforming medical coding faster than most people realize. Ambience Healthcare recently announced an AI model that outperforms physicians by 27% in medical coding accuracy. While this sounds threatening to coders, the reality is more nuanced.
What AI Does Well (And What It Doesn't)
AI excels at:
- Pattern recognition in clinical documentation:
- Consistent application of coding rules:
- Speed in processing routine cases:
- Compliance checking against current code sets:
But AI still struggles with:
- Complex clinical scenarios requiring judgment:
- Conflicting documentation that needs clarification:
- New or unusual conditions not well-represented in training data:
- Contextual understanding of physician intent:
The Smart Approach to AI Implementation
The practices getting the best results are using AI to augment human coders, not replace them. Here's what this looks like practically:
- AI handles routine cases: (outpatient visits, lab results, straightforward procedures)
- Human coders focus on complex cases: (surgical procedures, multiple diagnoses, unusual circumstances)
- Quality assurance remains human-driven:
- Exception handling and appeals require human judgment:
Patient Financial Engagement: The Revenue Stream You're Probably Missing
With patient responsibility continuing to grow (now averaging 30-40% of total practice revenue for many specialties), your approach to patient collections directly impacts your bottom line.
Digital Payment Strategies That Work
The data is clear: 68% of patients prefer to pay medical bills electronically. But it's not just about offering online payment, it's about making the entire financial experience seamless.
- Multi-Channel Approach: Text payments, email invoices, online portals, and mobile apps should all be part of your strategy. Different patient demographics prefer different channels.
- Payment Plan Automation: Flexible, automated payment plans increase collection rates by 10-30% compared to traditional billing. The key is making enrollment self-service.
- Transparent Cost Estimates: Patients who receive accurate cost estimates upfront pay 25-30% faster than those who get surprised bills. Investment in patient estimation tools pays for itself quickly.
Value-Based Care: The Long-Term Play
While fee-for-service cuts are painful now, the industry is moving toward value-based reimbursement models. CMS aims to have all Medicare beneficiaries in value-based care by 2030.
- Positioning Your Practice for VBC: The practices that will thrive in value-based care are already building the capabilities:
- Data Analytics Infrastructure: You need to track outcomes, not just procedures. This means integrating clinical and financial data into ways most practices haven't done before.
- Care Coordination Systems: Value-based contracts reward you for keeping patients healthy and out of hospital. This requires care management capabilities beyond traditional practice models.
- Quality Reporting Excellence: MIPS performance thresholds are staying at 75 points through 2028, but the measures are evolving. Getting quality reporting right now prepares you for more sophisticated VBC contracts later.
Your 2025 Action Plan
Following all that I've discussed, here's what I suggest you focus on:
Immediate Actions (Within 30 Days)
- Monitor your clean claim rate and denial patterns:
- Automate eligibility verification: if you haven't already
- Check previous authorization processes: for your highest-volume procedures You may arrange an independent, no-strings-attached audit here
- Instruct personnel on 2025 CPT code updates: for your specialty
Medium-Term Investments (Next 90 Days)
- Enhance the claim checking system: with AI technology.
- Utilize patient estimation tools: for enhanced financial participation
- Develop KPI dashboards: for regular performance tracking
- Assess AI-powered coding products: for common situations
Long-Term Plan (Second Half of 2025)
- Use value-based care competencies: with data analytics
- Create care coordination systems: for improved patient outcomes
- Improve denial prevention: through predictive analysis.
- Create sustainable telehealth billing systems:
The key argument
It's hard in 2025, but not impossible. The practices that will thrive are the ones that leverage technology but still maintain their attention to the fundamentals: good code, efficient workflows, and excellent patient experience.
The one thing that I most want you to remember is this: don't try to fix everything at the same time. Find two or three places where you can really make some headway, get those done well, and then expand outward from there. The health finance world will continue to evolve, but well-managed practices and decision-making based on fact will always manage to weather the storm.
What are the specific challenges you are facing as a result of these changes? I would recommend you begin with the areas where you can directly add to your revenue cycle, and work your way up to the more complex skills that will set your practice apart in value-based care.
Remember: no matter how many times the technology and the rules turn over, the principle is the same: you need to be reasonably and timely compensated for the good care that you provide. The rest is just a means to that goal.

