Overview of UnitedHealthcare Medicare Advantage Referral Requirements for 2026
From January 1, 2026, UnitedHealthcare (UHC) will be requiring its members who are signed up for Medicare Advantage HMO and HMO-POS plans to receive a referral from their primary care provider prior to them visiting most specialists.
This is one of the largest refinements of the referral policy that UHC has implemented in a very long while. Patients will receive more organized assistance with their care, and providers will need to follow new steps to ensure that claims are paid appropriately.
Why UnitedHealthcare Is Changing Medicare Advantage Referral Rules
UnitedHealthcare’s referring standards for the year 2026 aim at improving specialist-referral relationships with primary care doctors. In requiring a referral from patients, UHC aims at:
- Reduce unwarranted specialist referrals
- Improve communication between providers
- Avoid duplicate tests and procedures
- Ensure that members receive care that matches their overall health plan.
For patients, that shift will mean they will be seen by a primary care physician prior to visiting multiple specialists. For doctors, that will mean new guidelines governing scheduling, billing, and submitting claims.
UnitedHealthcare Specialists and Services That Do Not Require Referrals
Not all services will require referrals under the new policy. Patients will still be able to access the following specialists directly:
- Primary care providers
- Mental health providers
- Obstetricians and gynecologists
- Chiropractors
- Audiologists
- Oncologists
- Hematologists
- Nuclear medicine
- Neonatology
- Emergency medicine
- Nutrition services
- Podiatry
- Optometry
- Ophthalmology
- Optician services
- Radiology
- Therapeutic radiology
- Infectious disease
These exemptions ensure members can continue to receive urgent and routine care in critical areas without added administrative steps.
Referral Timeline for UnitedHealthcare Medicare Advantage in 2026
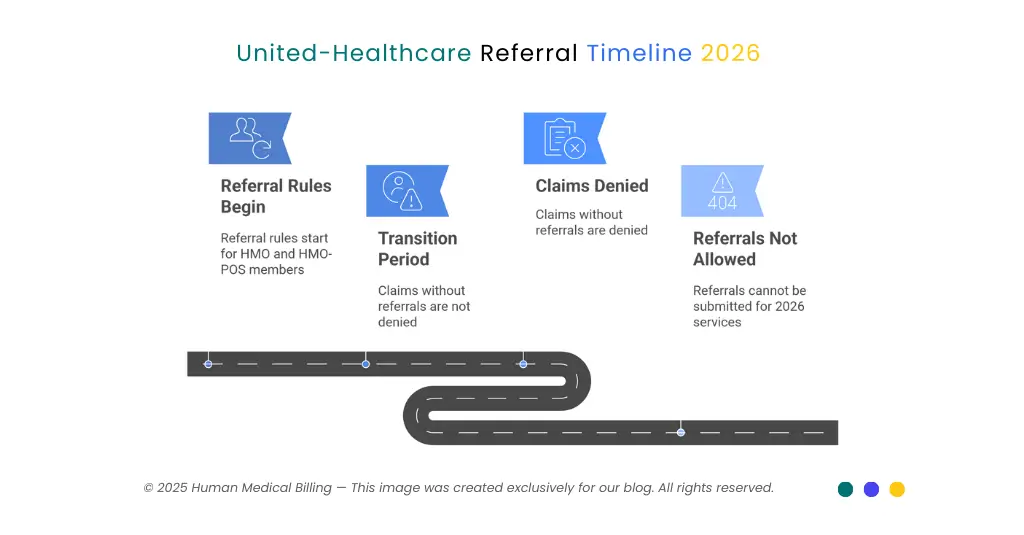
UnitedHealthcare has created a phased rollout to give providers time to adapt.
| Date | Referral Rule Detail |
|---|---|
| January 1, 2026 | Referral rules begin for Medicare Advantage HMO and HMO-POS members |
| Jan 1 – Apr 30, 2026 | Transition period, claims without referrals will not be denied |
| May 1, 2026 | Claims without referrals will be denied, provider is financially responsible |
| Before Jan 2026 | Referrals cannot be submitted for services dated in 2026 |
This timeline allows providers four months to establish referral processes before denials begin.
Plans and States Exempt from UnitedHealthcare Referral Requirements
These guidelines do not apply to all plans and members equally. The following are exempted:
- Institutional Special Needs Plans (SNPs)
- Erickson Advantage plans
- Michigan Integrated DSNP (H2247-005)
Members from California, Nevada, and Texas already need pre-authorizations for UHC Medicare Advantage, and those state mandates will not be shifting next year 2026.
Billing and Provider Compliance with UHC Referral Policy 2026:
Starting in May 2026, claims without referrals will not be accepted. Providers will have to pay the cost, and members are safe from extra charges.
Steps for Billing and Revenue Teams:
1. Eligibility checks:
Confirm referral requirements during scheduling.
2. Tracking of referrals:
Include verification of referrals while following pre-authorisation procedures.
3. Documenting:
Document referrals on the patient’s chart before you submit the claims.
4. Electronic submission:
Submit through the UHC Provider Portal. Track referrals.
5. Appeals and denials:
Prepare for referral-related denials and train staff on appeals.
The early 2026 transition offers a way to experiment with and perfect referral workflow at no expense.
Steps Providers Should Take to Prepare for UHC Referral Rules
Providers should begin planning now to avoid claim denials once enforcement begins. Key steps include:
- Identify members affected by the referral requirement
- Train scheduling and billing staff on referral verification procedures
- Create referral request protocols with primary care providers
- Set up electronic tracking through practice management systems
- Educate patients about referral rules to prevent confusion
What Patients Should Know About UnitedHealthcare Medicare Advantage Referrals
- You will need referrals for most specialists from 2026 onward.
- Begin with your family physician if you need a specialist.
- Ensure that your provider refers you to UnitedHealthcare prior to your visit.
- You won’t have to pay if you do not have a referral. Otherwise, your wait will be longer.
- In Nevada, California, and Texas, referring procedures are already in place that will not be modified.
Frequently Asked Questions About UHC Medicare Advantage Referrals 2026
Yes. Most HMO and HMO-POS members will need referrals. PPOs and certain special needs plans are exempt.
Specialists such as mental health, OB/GYN, oncology, radiology, and emergency medicine are exempt.
Yes. Starting May 1, 2026, claims will be denied if referrals are missing, and providers will be financially liable.
No. Patients are protected from balance billing.
California, Nevada, and Texas already require referrals, and their rules will not change.
Conclusion
The new UnitedHealthcare Medicare Advantage referral requirements for 2026 will affect both patients and providers. Members will need to follow new steps to see specialists, and providers must adapt billing and scheduling processes to avoid claim denials.
At Human Medical Billing, we help healthcare organizations manage payer changes, set up referral tracking, and reduce the risk of denied claims.
Contact us today to prepare your workflows before May 2026.

