What is the real price of prescription drugs? A physician, a patient, and an employer would probably have three different answers. Pharmacy Benefit Managers (PBMs), which acted in a "black box" for years, were able to negotiate behind closed doors; PBMs kept rebates for themselves; now the U.S. Government intends to "turn the light on".
In response to the proposed rule by the U.S. Department of Labor's Employee Benefits Security Administration (EBSA) that requires Pharmacy Benefit Manager (PBM) transparency to be enforced as of January 29, 2026, the rule was formally published in the Federal Register on January 30. The target of this new regulation are the intermediaries involved in the sale of pharmaceuticals. The goal is to reduce the costs to self-insured employers and patients.
So why should this proposed rule affect a medical practice or a hospital? Higher priced medications consume all of the financial resources of the entire healthcare system. When patients are unable to purchase their prescribed medications, patients will either stop taking the medications or take them sporadically; both actions can result in poor patient health and added administrative burden for your staff.
At Human Medical Billing, we monitor these changes to your revenue as they occur. We will now explain the details of this proposed rule.
What are the New PBM transparency requirements?
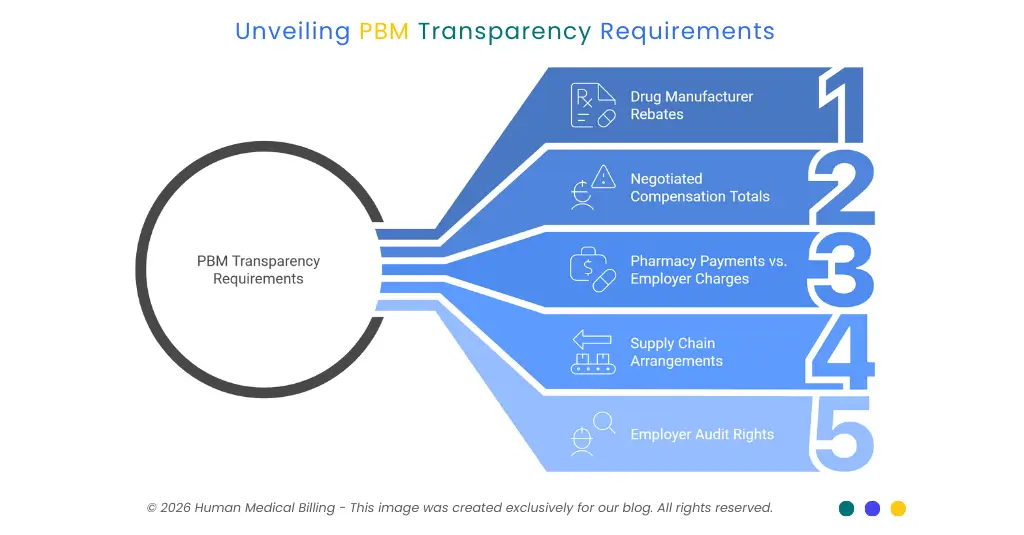
The proposed rule emphasizes accountability. The rule requires that any PBMs who provide services to ERISA self-funded group health plans be required to disclose specific financial information directly to the plan's fiduciary. Examples of the types of information that will be disclosed by the PBMs include rebates made to the drug manufacturers and payments made to pharmacies compared to what the employer paid for those same drugs.
Here are some examples of the specific types of financial information that must be provided by PBMs under this rule:
- Full details on drug manufacturer rebates.
- Negotiated compensation totals.
- Amounts paid to pharmacies versus what the employer was charged.
- Arrangements with other parties in the supply chain.
Employers will have the ability to audit the disclosure of this information as part of the new rule. This is a significant change since many employers have been prohibited from examining how much they were being charged for their prescriptions as a result of the restrictive nature of many PBM contracts.
Why is the Labor Department Acting Now?
Pharmaceutical manufacturers have seen an increase in public and legislative scrutiny concerning their supply chain. As well as other players, PBMs such as OptumRx, CVS Caremark and Express Scripts hold significant portions of the marketplace share. In response, lawmakers are claiming that PBMs drive up the cost of drugs by utilizing a strategy called "spread pricing".
Spread pricing is defined as the amount a PBM charges a health plan for a drug, minus what the PBM reimburses the pharmacy for the same drug. Essentially, a PBM keeps the "spread" for themselves as profit. To help remove these "hidden" markups from the process, the Labor Department has proposed requiring PBM's to be transparent with respect to their rebate on drugs, their arrangement with pharmacies, and how much they pay pharmacies for each prescription.
What is the 2026 PBM Transparency Rule?
The 2026 proposed rule from the U.S. Department of Labor requires PBMs to provide rebate information on every drug to any self-insured employer who utilizes one of their PBM services, and also requires them to provide all pharmacy reimbursement information to those same employers. This rule would allow employers to conduct audits of the PBM services they use, to ensure that the prices charged for drugs are correct and that employers are getting fair drug prices for their employees.
How Hidden Costs Affect Your Revenue Cycle
You may assume that prescription drug costs are unrelated to your medical billing. However, as high-cost drugs increase deductibles and ultimately leave little for your patients' other care expenses (ie. physician visits/procedure) after spending all of their deductible amount at the pharmacy; the burden of additional collections in your medical accounts receivable is increased.
In turn, your medical billing staff will spend more time collecting debt that your patients are unable to pay for, creating an even larger burden in your medical billing department.
At Human medical billing, we see this trend often. The ability to be transparent with all pricing will help to stabilize the healthcare marketplace. Employers who realize savings from lower pharmacy benefit rates will be able to provide better coverage for medical services. Ultimately, this will result in less denied claims and improved healthcare revenue cycle management services.
Key Facts About the PBM Market
To understand the scale of this issue, look at the data.
| Metric | Detail |
|---|---|
| Market Share | Three PBMs control about 80% of the market. |
| Proposed Change | Full disclosure of all rebates and service fees. |
| Audit Rights | Employers can verify PBM data for accuracy. |
| Target Group | ERISA self-insured group health plans and their fiduciaries. |
The Pharmaceutical Care Management Association (PCMA), which defends the current model, argues PBMs help lower costs for health plans. Critics argue that cost savings often do not go to either the employer or the patient. Therefore, the new PBM transparency requirements represent the first opportunity for evidence-based proof to resolve this long-standing argument.
The Link Between Transparency and Medical Coding Services
Accuracy is essential to the delivery of healthcare. Employers also rely on accurate information regarding their employee health plans just as you rely on accurate medical coding services to be able to collect a payment.
If a PBM provides an invoice price that does not reflect the actual payment made by the pharmacy, then the employer has been misled into believing they have purchased value; when, in reality, they have paid the PBM for profit.
More transparent data will allow for improved plan designs. Your practice may find that self-insured employers will begin asking for additional details in their reporting. This is another example of how artificial intelligence (AI) medical billing software can help track changes in a timely manner.
Common Questions About PBM Rules
These requirements help lower the total cost of care. When drug prices are transparent, it is easier for doctors to prescribe affordable medications that patients will actually take.
Under the new Labor Department proposal, employers gain a legal right to audit the accuracy of PBM disclosures. This prevents PBMs from hiding fees in complex contracts.
Yes. By forcing PBMs to pass rebates back to the plan or the patient, the "list price" of drugs should decrease over time.
Managing the Shift with Human medical billing
With the trend of transparency continuing within the healthcare sector (i.e., all costs being made available to consumers), your practice needs to be ready for the increased need for clarity from both the PBMs and Hospitals.
Our team will handle the "black box" of Insurance & Pharmacy Benefits to allow you to focus on patient care. We have a number of solutions to help keep your cash flow flowing:
- Medical Credentialing Services to get you in-network with the correct plans
- Denial Management Services to prevent your practice from losing money due to denied claims
- Reliable Medical Billing Services which adjust as federal regulations continue to evolve.
How Our Services Work
We don't just process claims. We analyze the entire cycle. Here is how we help:
- Analysis: We look at your current payer mix and identify trends.
- Coding: Our team ensures every code is accurate.
- Submission: We send claims quickly using the latest technology.
- Follow-up: We handle the "difficult" payers so you don't have to.
Visit our about us page to see our history of helping providers. You can also read our success stories to see how we have improved revenue for practices like yours.
Next Steps for Providers
As of now the Department of Labor is still in its comment phase regarding the proposed rules. These rules will not be finalized until after the comment period ends; however, there is an unmistakable trend in both parties within Congress to support more oversight for Pharmacy Benefit Managers (PBMs).
Here is what you need to do:
- Review your existing contracts: Check to see if your current contracts are impacted by any changes made by PBMs.
- Educate your patients: Explain to your patients why they may experience changes in the cost of medications.
- Update your billing software: Be sure your billing software will allow you to submit required reports related to the proposed rules.
If you have questions as to how these proposed rules will impact your bottom-line financially, please review our Xpert Billing Blog regularly for updates on medical laws and other financial news. We also provide answers to commonly asked questions on our FAQ’s page.
The Larger Perspective
The push for the implementation of PBM transparency provisions is just one example of the greater efforts being made to create a more equitable healthcare system. When the pharmacy side of the equation is transparent, it forces the medical side to be equally transparent.
This is a benefit for all providers who are honest and work to deliver quality care. This creates a level playing field. It also makes sure that monies intended for patient care are utilized for that purpose.
Human Medical Billing is excited to support this transition. We believe that clarity in billing equals quality medicine. If you are prepared to see how a business partner can make a difference in your practice, please go to our contact us page today.
Summary of the Proposed Rule
- Who is affected: PBMs serving ERISA self-insured group health plans and the fiduciaries responsible for those plans.
- What is required: Detailed reports on all money moving through the PBM.
- Why it matters: It exposes hidden fees and lowers drug costs.
- Status: Proposed by the Labor Department in January 2026.
Stay tuned, these new PBM transparency mandates are only a first step. Once more information is publicly available, the ways in which we bill, code and collect will be improved.
Help us make your practice more resilient. We can provide you with medical coding services or denial management services. We want to make certain you receive payment for the hard work you put into your patients' care each and every day.
FREE DOWNLOAD: The 2026 PBM Audit Readiness Checklist
(Disclaimer: By providing your email, you agree to receive our weekly newsletter. You can unsubscribe at any time.)
Thank You!
Your download has started.

Contact Human Medical Billing to schedule a compliance readiness review or learn more about our end-to-end billing and regulatory support services.

