The new Medicare rule for 2026 removes 285 musculoskeletal surgical procedures from the Medicare Inpatient-Only (IPO) List starting January 1, 2026, allowing those procedures to be billed in outpatient settings, including ASCs. The IPO list will be removed entirely by January 1, 2028.
A significant change in Medicare policy has been finalized, and it will significantly alter how your hospital handles surgery billing over the next two years.
In the Calendar Year 2026 Outpatient Prospective Payment System (OPPS) Final Rule, CMS stated that it would eliminate the Medicare Inpatient-Only List completely. This is sooner than most had anticipated.
For years, the IPO list required hospitals to have patients stay at least one night after performing some of the more complex surgeries listed on the IPO list. When you billed these codes as outpatient services, Medicare denied those claims. Now, that protection will be gone. While this allows greater flexibility for hospitals and ASCs to choose where their patients are treated; it also subjects those facilities to increased risk of denials by other third-party payers who will likely aggressively try to direct those patients to lower cost sites of service.
Below is an accurate summary of the OPPS Final Rule and what you can do to protect your facility's revenue cycle.
The CMS Phase-Out Plan (2026–2028)
CMS was going to eliminate the list of Inpatient-only (IPO) procedures by 2029, however the final rule has accelerated this timeline. The agency is planning to phase out the IPO list over a three year time frame which ends on January 1st, 2028.
New Timeline for Elimination of IPO Procedures:
1. January 1, 2026:
CMS eliminates the first 285 musculoskeletal and other related musculoskeletal codes from the IPO list. This includes complex spine and orthopedic surgical codes.
2. 2027:
CMS will begin eliminating the remainder of the procedure codes in groups.
3. January 1, 2028:
The Medicare Inpatient-Only List will no longer exist.
Why CMS Is Doing This
The largest factors driving the trend toward outpatient treatment are cost efficiency and flexibility. Generally, providing a patient with outpatient services is cheaper for the Medicare program than treating them as an inpatient at a hospital.
A few conservative policy organizations, including the Paragon Health Institute, advocate for this type of transition, and suggest that site neutral payment will result in lower cost to taxpayers. The Ambulatory Surgery Center Association (ASCA), also advocates for this change, citing that site neutral payment gives surgeons the option to provide care at the best location for their patient’s health needs rather than being limited by billing considerations.
The Opposition: Safety Concerns
Hospitals are fighting back against this proposed rule; the American Hospital Association (AHA), specifically, has come out in opposition to the blanket removal of all surgical procedures from the list.
The AHA's Senior Vice President for Public Policy, Ashley Thompson, stated that "the AHA opposes this proposal." The AHA is cautioning that the removal of these surgical procedures on a group basis is premature because it does not take into account the important distinctions between a full service hospital and an outpatient center.
Orthopedic surgeons are also cautious about this potential change; as the AAOS has pointed out, flexibility with regard to insurance coverage can be beneficial to patients; however, this may create undue pressure on physicians to send high-risk patients to outpatient centers prematurely.
The Hidden Danger: Denials and "Site Neutrality"
This is probably the weakest part of your Revenue Cycle.
Medicare can still say that a surgery may be an outpatient surgery, but this doesn't mean Medicare Advantage or commercial insurance companies have to reimburse you for the surgery in the hospital.
After CMS took TKA off the IPO List about three years ago, a lot of payers began denying all inpatient TKA claims and said they had to be billed as outpatient surgeries. We anticipate a similar trend for the 285 codes going into effect in 2026.
If your team continues to submit these surgeries as inpatient with inadequate supporting medical necessity documentation, your denials will rise significantly. Your team needs to proactively work with denial management services so you can deal with what will be a significant amount of friction between your organization and the payers looking to cut their cost.
How This Affects Your Operations
Immediate changes are needed in both your front and back office due to the elimination of the Medicare Inpatient-Only List.
The authorization process is critical: All surgeries require verification by your staff as to what is the approved site of service prior to scheduling.
Correct coding: The 285 removed surgical procedure codes will have new status indicator assignments in the CY 2026 addenda, and your medical coding services team must be trained on this update to avoid denied claims.
Documenting: If a physician documents that a patient’s surgery required an in-patient hospital stay when it can actually be performed at an out-patient center due to the elimination of the Medicare In-Patient Only list; the physician must document clinical rationale such as comorbidities or other safety risks to support in-patient admissions.
Any errors made during this transition may cost you thousands of dollars in lost revenue due to write-offs. At Human Medical Billing, we monitor all regulatory updates affecting our clients. Our medical credentialing services also help providers expand their privileges to new outpatient centers as volumes shift.
Quick Look: The 2026 Transition
| Feature | Current Status (2025) | New Rule (2026) |
|---|---|---|
| IPO List Status | Active (~1,700 codes) | Phase-out begins (Ends Jan 1, 2028) |
| Primary Change | Codes restricted to Inpatient | 285 codes (mostly ortho/spine) allowed Outpatient |
| Payer Behavior | Follows IPO List | High Risk: Payers may demand outpatient use |
| Documentation | Standard Inpatient criteria | Crucial: Must prove need for inpatient stay |
Steps to Protect Your Revenue
There is a very small amount of time remaining prior to implementation of this regulation at the beginning of next year.
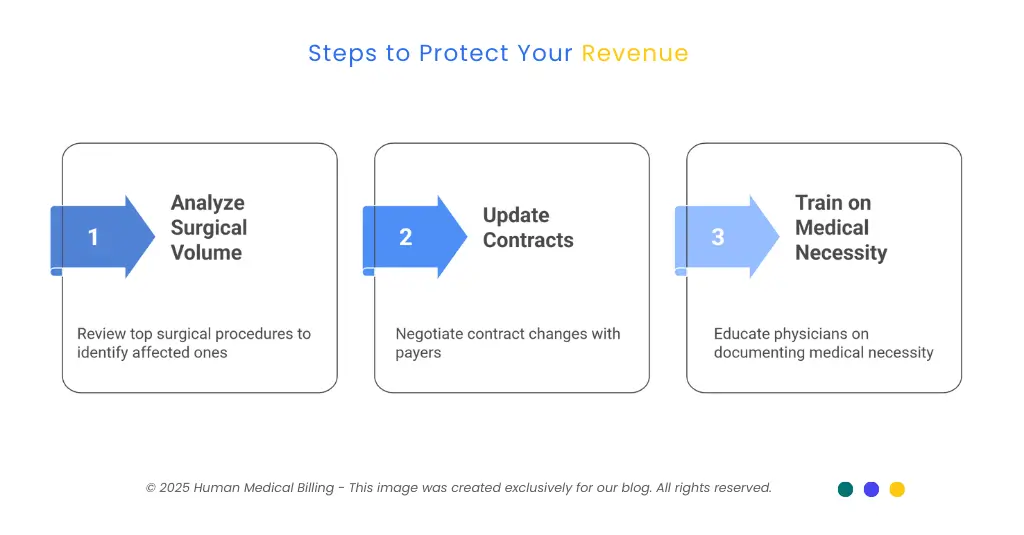
1. Analyze Your Volume:
Evaluate Your Volume Review the Top 50 Surgical Procedures you have performed over the last year or longer. Identify those that will be removed by CMS in 2026. In the event your most common surgical procedures are among those identified by CMS for removal, then changes must occur in your billing process for these specific surgeries.
2. Update Your Contracts:
Negotiate Changes in Your Contracts Contact all Commercial and Medicare Advantage Payers to whom you currently bill. Determine what policies they intend to follow in regard to the 2026 IPO removals (e.g. outpatient). Document the responses from each payer to include any mandates for outpatient in writing.
3. Train on Medical Necessity:
Educate Physicians Regarding Medical Necessity Documentation Physicians will need to understand that "clinical judgment" alone may not result in a claim being processed for payment. Physicians will need to provide documentation supporting why the clinical judgment was made. Medical accounts receivable services can clean up old claims, but getting the documentation right upfront is far cheaper.
History: The 2021 Reversal
The biggest threats to independent practice and hospital are regulatory changes. Regulatory changes can cause cash flow issues when the rules change.
Human Medical Billing helps to stabilize the financial instability caused by regulatory changes. Our medical billing company provides full-service revenue cycle management and helps to protect your revenue from the effects of CMS updates with timely response to CMS updates.
Whether it is using ai medical billing to detect site-of-service errors or whether it is managing complex appeal issues, we will help to maintain your revenue stability.
If you are concerned about the 2026 changes, please review our FAQs or view our success stories. We have assisted numerous providers through the previous TKA changes, and we will assist you with the upcoming changes.
Frequently Asked Questions
The Phase-Out of the Inpatient-only List begins on January 1, 2026. CMS has also finalized its plan to completely remove the list by January 1, 2028.
CMS is eliminating 285 mostly musculoskeletal procedures from the Inpatient-only List. These eliminated procedures will be billable in Hospital Outpatient Departments. CMS is adding 271 of those procedures (and additional procedures) to the Ambulatory Surgical Center (ASC) Covered Procedure List for 2026.
Yes. Although this is a Medicare Rule, most Commercial Payers and Medicare Advantage Plans follow the same billing guidelines as CMS. Expect the elimination of these procedures from the Inpatient-only List to lead to denials of Inpatient Claims for these surgeries.
CMS believes it is safe for many patients, but not all. The AHA and other groups argue that safety depends on the individual patient. Physicians must carefully screen candidates for outpatient surgery.
Next Steps
The elimination of the Medicare Inpatient Only (IPO) list creates both risk and opportunity for your organization. On one hand you can potentially increase volume in your ambulatory surgery center; however, this could create a higher risk for denials when treating patients in your hospital.
Do not be unprepared for changes coming in 2026. Click the "Contact Us" link on our website today to have the team at Human Medical Billing review your surgical coding and authorization processes. Our staff will demonstrate to you how our services help protect your payment in an ever-changing environment.
Bookmark the Xpert Billing Blog as we update information regarding new CMS regulations. As an educational resource, we will provide explanations that are easy to understand regarding the complex rules that you need to follow to allow you to continue providing quality patient care.

