Introduction: The Changing Face of Medicare Advantage
2025 brings revolutionary change in the documentation, coding, and follow-up requirements for MA health plans and care providers when documenting the diagnosed conditions of their patients during home visits.
These sweeping Medicare Advantage home visit diagnosis changes are designed to improve accuracy, prevent improper upcoding, and improve care pathways to America's rapidly growing MA population, now more than 32 million beneficiaries (according to CMS 2024 statistics).
Educating physicians, practices, and billing staff on these reforms will be critical not just for compliance, but for clinical quality, financial success, and long-term credibility with payers and patients.
Background: Why Focus on Home Visit Diagnoses?
MA employs providers who treat Medicare beneficiaries and compensate the providers "risk adjusted" for patient panel severity or illness.
Home health risk assessments (HRAs) were a valuable tool in the past that enabled primary care providers (PCPs) and visiting clinicians to detect undiagnosed or poorly managed chronic disease (e.g., heart failure, COPD, or diabetes) in frail or homebound patients.
But as analyzed by the Office of Inspector General (OIG) and investigative journalists:
- Certain home visit diagnoses were not validated by follow-up visits but cost more MA plan coverage.
- In the years 2016–2022, up to $50 billion in payments were at risk due to insufficient documentation or "chart review only" diagnoses, according to CMS.
- Government audits in 2024 revealed that more than $7.5 billion was reimbursed for diagnoses that were only on chart review and had no accompanying in-person clinical visit or follow-up.
Hence, Medicare Advantage home visit diagnosis reforms have been implemented to verify that all coded diagnoses capture true current medical need and proper care action.
In-Depth: 2025's Most Important Policy Shifts
Medicare Advantage plans, under new CMS regulations, and the industry have pledged to a higher level of home visit risk assessments.
Below is the most critical change affecting you:
| Topic | Previously | New 2025 Reforms |
|---|---|---|
| Setting | Home/any visit | Still permitted at home, but are subject to higher standards. |
| Documentation | Any diagnosis on chart | Should be associated with real-time or telehealth (subject to authorization) face-to-face interactions and should satisfy clinical requirements. |
| Follow-up | Not required | Shall continue to follow-up new or significant diagnoses. |
| Chart Reviews | Used for risk scoring | Independent chart review diagnoses are no longer allowed to accept risk payment. |
| Annual Audit | Rare | Routine audits expected—plans must demonstrate care provided matches coded diagnoses. |
| Care Pathways | Not always tracked | New diagnosis must be followed by ongoing care coordination, management, or referral. |
Clinical Best Practices: Shaping Your Workflow
As a general practitioner or practice manager, the following is what Medicare Advantage home visit diagnosis reforms mean for your day-to-day business:
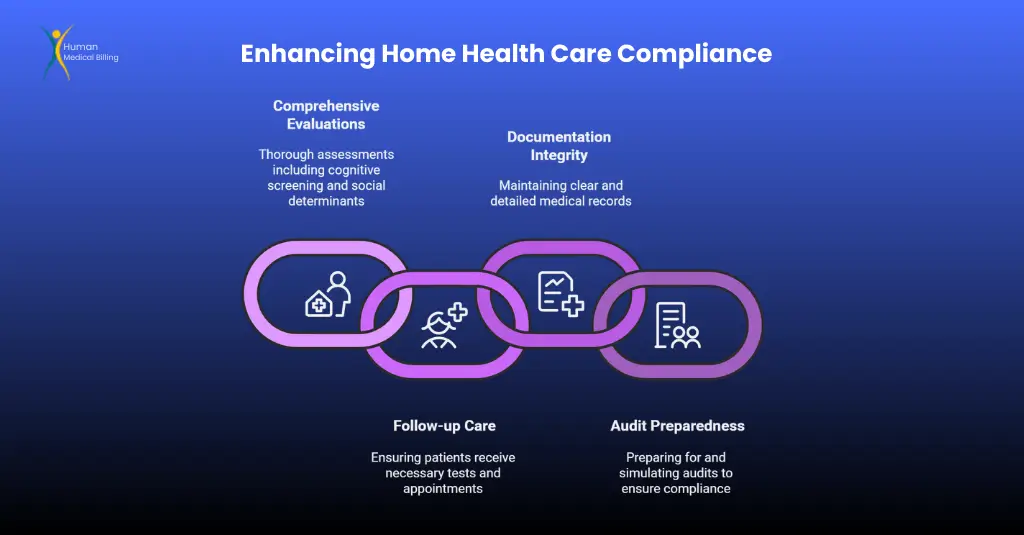
1. More Extensive Home Visitation Evaluations
Home Health Risk Assessments (HRAs) must be as thorough as a clinic-based Annual Wellness Visit (AWV):
- Include cognitive impairment screening, risk factors, medication reconciliation, and social determinants of health assessment.
- All the components should be recorded in the EMR/EHR for billing and compliance audit.
2. Follow-up Is Necessary
For each new chronic or acute disease diagnosed, patients must be:
- With needed lab/imaging tests, specialty appointments, or chronic disease management programs.
- Direct instruction for next steps either for in-person follow-up or continued telehealth contact (when CMS standards permit).
3. Documentation Must Be Air-Tight
Chart notes need to:
- Clearly indicate the method of assessment, diagnostic reasoning, and clinical significance.
- Offer any follow-up or subsequent treatment arrangements.
- Tie the diagnosis to a face-to-face visit or telehealth encounter by a trained provider - a chart review is not enough.
4. Preparing for Audits
- Expect repeated requests for supporting documentation from MA contracts or network partners.
- Identify and execute internal processes or use a third-party like Human Medical Billing, to perform active audit simulations and detect common documentation errors before payers.
Scenario Spotlight: What Happens If…
Scenario 1: OSA Detected During Home HRA
Earlier:
Home visits provided to patients and documented as "possibly" having obstructive sleep apnea on sleep history. Diagnosis is coded; insurer pays more, with no test or follow-up prescribed.
2025 Forward:
This diagnosis is then supplemented by:
- Referral for sleep study in 60 days.
- Clinical interpretation of test results.
- Treatment plan and ultimate diagnosis co-documented in the medical record.
Result:
If these steps are not taken, payment for OSA risk adjustment can be taken away, potential audit flag.
Scenario 2: Home Visit Reveals Uncontrolled Diabetes
The home visit nurse detects high blood glucose and concerns regarding uncontrolled diabetes.
Under reforms, these new diagnoses require:
- Expedited PCP follow-up or endocrinology referral
- Current drug regimen
- Clear documentation that the patient has been taught and will be observed for improvement
Telehealth and Home Visits: A Point of Transition
The 2020–2024 public health emergency expanded telehealth coverage, including home visits. But starting April 1, 2025:
- Telehealth home visits will be more restricted - only permitted in rural/shortage populations or for specific modalities by CMS.
- Telehealth diagnoses are still "clinically robust" (video, not audio-only, where possible), and documentation/follow-up rules are still in effect.
Data Points: Medicare Advantage Growth & Overpayment Risks
| Year | MA Enrollment (Millions) | Improper Payment Risk (USD, Billions) |
|---|---|---|
| 2022 | 28.4 | $12.4 |
| 2023 | 30.8 | $15.3 |
| 2024 | 32.8 | $16.6 |
Audits found payments to some plans of more than 10% that traced to diagnoses revealed through chart reviews or home visits with no follow-up care.
OIG, HHS, 2024
How Reforms Affect Your Revenue Cycle
Well-documented, efficient billing is now priority number one.
Non-compliance gaps can cause:
- Lost payment for rightful care
- Long, punitive audits
- Cashflow disruptions and revenue cycle delays
Human Medical Billing offers advanced healthcare revenue cycle management services to:
- Capture errors before they hit payers
- Track policy updates and requirements
- Improving on-time payment per compliant service provided
Physician FAQ: Real Questions for 2025
Yes, if well documented, with in-office or live telehealth evaluation, and followed up on in your practice or referral base.
Full HRA forms, patient contact reports (video/audio logs where allowed), up-to-date care plans, and follow-up services or consult records.
Best practice is 30–60 days with documentation in the EHR, but individual MA plans may have stricter requirements.
Having a business partner in medical billing services like Human Medical Billing can provide chart audits tailored to your needs, staff training, and EHR system assessments to address issues in a timely manner.
The Role of Medical Billing Professionals
It is a delicate navigation through the reforms and compliance is high-stakes.
In case you need assistance with medical accounts receivable services, guidance on billing and automation, Human Medical Billing is your go-to advisor in this dynamic environment.
We're not vendors - we're business partners, helping you through even policy changes. Read our success stories or call us to learn how we navigate even the toughest policy changes for your practice.
Real-World Application: Smart Steps for 2025
- Review HRA Protocols: Revise all HRA and home visit processes to fully integrate with enhanced AWV standards.
- Team Training: Educate all billing and clinical personnel on revised follow-up and documentation procedures for MA home visit diagnosis revisions.
- EHR Optimization: Utilize personalized templates and "smart fields" within your EMR to ask for necessary information on each home visit.
- Routine Self-Audits: Conduct monthly "test audits" with your billing partner - find gaps before payers do.
- Leverage Technology: Leapfrog with AI and automated auditing (such as Human Medical Billing's offerings) to identify coding and payment risk patterns.
Conclusion: Opportunity Under the Challenge
The launch of Medicare Advantage home visit diagnosis reforms in 2025 is a shift in the health system but offers new channels for high-quality practices:
- Greater patient trust with more care
- Removal of abusive and fraudulent payment
- Intelligent, cost-effective medical billing and revenue expansion for compliant segments
By embracing best practices aggressively and working with an experienced expert like Human Medical Billing, you can turn reform into a competitive advantage.
For further help with adapting to 2025's new reality, visit our How Our Services Work page or phone our staff today.
Tune in for additional expert advice on the Xpert Billing Blog, or get in touch with Human Medical Billing to get your revenue cycle successfully up and running securely.

