The market for medical billing outsourcing is flourishing, and its global value is set to hit $54.17 billion by 2034. If your health organization is witnessing growing administrative work and complicated payer regulation, selecting a suitable medical billing company is more necessary than it’s ever been before.
Your choice of a medical bill firm is a make-or-break for your practice’s finances, whether your practice experiences returns or is overwhelmed by expense-deny claims.
What Makes the Best Medical Billing Company Stand Out
The best medical billing company integrates industry knowledge, advanced technology, and clear procedures to produce quantifiable outcomes.
As more than 70% of healthcare professionals are now sending their billing work elsewhere, comprehension of major differentiators becomes critical.
Industry-Leading Performance Metrics
Top-tier billing companies maintain exceptional performance standards. The industry benchmarks include:
- Clean claims rate above 95%
- First pass resolution rate of 95% or higher
- Net collection rate between 95-98%
- Days in accounts receivable under 30-45 days
Companies like Human Medical Billing, which have been around for more than 20 years and are A+ BBB accredited, continually achieve these outcomes consistently, utilizing specialized knowledge and tried-and-proven techniques.
The Financial Consequences of Your Decision
Selecting the best medical billing firmdirectly affects your bottom line. According to studies, successful medical billing organizations can boost revenue by 15-25% and administrative costs by up to 30%.
Poor billing decisions cost practices significantly:
- 15-20% of statements are denied outright on initial submission for error
- Averages of $125,000 per year loss for inefficiencies of billing
- 42% of billers are yet to implement automation, growing performance gaps
Essential Criteria for Choosing the Best Medical Billing Company:
1. Specialty-Specific Experience and Certification
Your best medical billing companion is well-versed in the special demands of your specialty. Specialties have special coding challenges:
- Cardiology requires expertise in complex procedures and device coding. Primary care is E/M coding and preventive medicine. Surgery demands knowledge of the bundled procedures and modifiers.
- Seek out businesses that employ AAPC or AHIMA certified coders. These credentials help ensure that your billing staff is up-to-date on the latest coding rules, such as the ICD-11 conversion preparation.
2. Technology Integration and EHR Compatibility
Modern billing requires technology that integrates well. The top medical billing company utilizes your existing systems rather than requiring you to pay costly changes in software.
Main technology features are:
- Integration with 25+ EHR systems (like leading companies offer)
- Live eligibility checking to prevent denials
- Pre-submission automated claim scrubbing to capture errors
- Advanced reporting for performance tracking
Companies that require specific proprietary software should raise red flags. This often indicates inflexibility and potential hidden costs.
3. Transparent Pricing and Contract Terms
| Pricing Model | Range | Best For |
|---|---|---|
| Percentage-based | 4-8% of collections | Small to medium practices |
| Per-claim fee | $3-8 per claim | High-volume practices |
| Hybrid model | Combination of above | Complex billing needs |
Pricing transparency separates reputable companies from problematic ones. The most common pricing models include:
Avoid companies offering unusually low rates below 4%, as this often indicates corner-cutting that compromises quality. The best medical billing company provides transparent pricing without hidden fees for claim resubmission or reporting.
4. Compliance and Security Standards
Medical billing compliance is not negotiable. Your selected firm should show rigid adherence to:
- HIPAA guidelines on safeguarding patient information securely
- Security provisions under HITECH
- State-specific billing regulations
- Medicare and Medicaid compliance standards
Request documents regarding their programs on compliance, such as periodic audits, training records on staff, and security certification.
Red Flags to Avoid When Choosing a Medical Billing Company
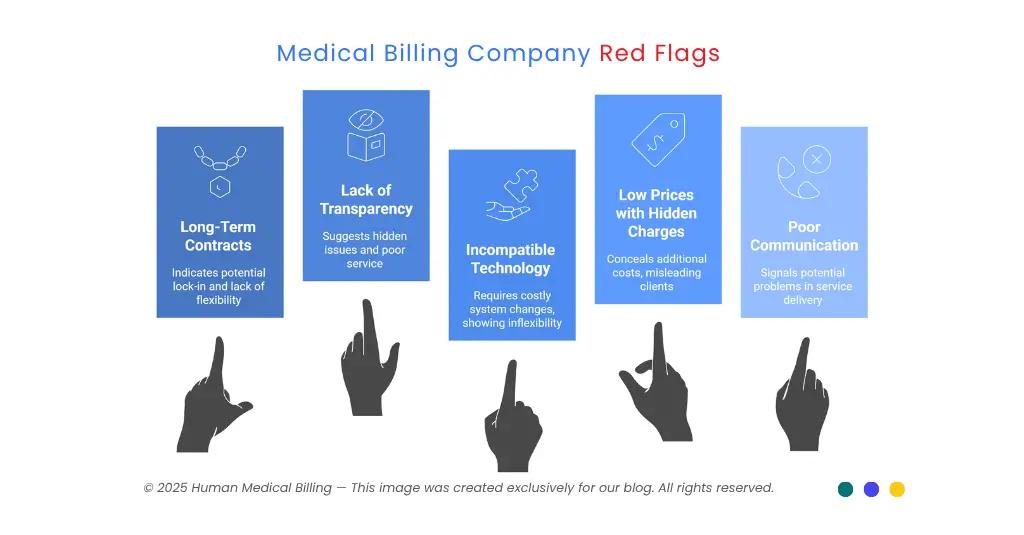
Warning Signs of Poor Service Providers
Several red flags indicate you should avoid certain billing companies:
Requirements for long-term contracts without flexibility are often a sign that the companies use lock-in, not performance. A top medical billing company provides month-to-month contracts, which reflect that they have faith in their quality service.
Failure to be forthcoming in reporting or providing client references indicates potential problems. Reputable companies have no problem providing client contacts and performance data.
Compatible technology needs compel costly system changes to signify inflexibility. Quality providers are flexible enough to accommodate your current infrastructure.
Challenging advertising with very low prices frequently conceals additional charges. Always request specific price information.
Signs of Poor Performance and Communication
Poor communication indicates trouble ahead:
- Slow replies to questions or problems
- Inability to generate system-generated reports
- Lack of submission of daily activity reports
- Negative client reviews along with mixed responses
The Evaluation Process: Step-by-Step Guide:
1. Phase 1: Initial Assessment and Requirements
Begin by specifying just what your practice needs:
- Volume analysis: Track your monthly claim volume and specialty mix. This informs the appropriate staffing and price models.
- Previous performance baseline: Enter your current figures like denial rates, days in A/R, and collection percentage. These provide comparison baselines.
- Technology requirements: List your current EHR, PM, and reporting needs. Make sure they will work with possible partnerships.
2. Phase 2: Vendor Research and Screening
Research potential partners thoroughly:
- Check credentials: See certificates, licenses, and evidence of compliance documentation. Look at Better Business Bureau ratings and licensing status.
- Reference checks: Call a number of existing customers in similarly situated practices and specialities. Ask specific questions about performance, communications, and resolution of issues.
- Financial stability: Review company financial health and longevity. Established companies like Human Medical Billing with 20+ years of experience offer greater stability.
3. Phase 3: Proposal Evaluation and Comparison
| Evaluation Criteria | Weight | ABC Medical | XYZ Healthcare | Human Medical Billing |
|---|---|---|---|---|
| Specialty experience | 25% | 7 | 6 | 9 |
| Technology compatibility | 20% | 8 | 5 | 9 |
| Pricing transparency | 20% | 6 | 7 | 9 |
| Performance guarantees | 15% | 5 | 8 | 8 |
| Client references | 10% | 7 | 6 | 9 |
| Contract flexibility | 10% | 4 | 5 | 10 |
| Weighted Total | 6.4 | 6.2 | 9.0 |
Score each criterion on a 1-10 scale and calculate weighted totals for objective comparison.
Key Performance Indicators to Monitor:
1. Revenue Cycle Metrics
Monitor these key KPIs to track the performance of your billing company:
- Net Collection Rate: Measures payments received against allowable charges. Industry benchmark is 95-98%.
- Days in Accounts Receivable: Days between service date and date of payment, average. Shoot for below 30-45 days.
- Clean Claim Rate: Percent of claims that are taken on the first submission. Aim for 95%+.
- First Pass Resolution Rate: Claims resolved without rejection on the initial submission. Industry standard is 95%.
2. Quality and Efficiency Indicators
- Denial Rate: It should be kept under 5-8% for peak efficiency. Monitor denial reasons to detect systemic problems.
- Charge Lag: Period between service date and submission date of the claim. Reduce to enhance cash flow.
- Cost to Collect: Total bill collection cost per collected dollar. Industry range is between 3-7%.
Technology Trends Shaping Medical Billing in 2025
1. Artificial Intelligence and Automation
Medical billing with AI is revolutionizing the process. Advanced systems today automate:
- Coding assistance with 99%+ accuracy rates
- Claims scrubbing to prevent denials
- Prior authorization tracking and management
- Payment posting and reconciliation
Companies that provide AI medical billing services provide significant competitiveness through increased accuracy and fast process.
2. Cloud-Based Systems and Real-Time Analytics
Modern billing platforms offer:
- Real-time eligibility verification to prevent coverage issues
- Advanced analytics dashboards for performance monitoring
- Mobile access for on-the-go practice management
- Automated patient communication for payment collection
3. The Importance of Specialty Expertise
Why Generic Billing Falls Short:
Revenue cycle management services in healthcare require significant specialty expertise. Generic billing approaches often result in:
- Higher denial rates from incorrect coding
- Missed revenue opportunities from unbilled services
- Compliance risks from specialty-specific regulations
- Poor patient experience from billing errors
4. Specialty-Specific Requirements
Medical credentialing services also differ significantly across subspecialties as well as primary care. Denial management services need education on the payer-specific criteria per specialty.
Medical coding services have to consider procedure-specific guidelines and the pattern of modifier usage specific to every speciality.
5. Contract Negotiation and Terms
The leading medical billing firm offers fair, understandable terms of engagement such as:
- Scope of service definition: Detailed definition of services that are included and exceptions.
- Performance metrics and guarantees: Specific KPI targets and remedies for underperformance.
- Data protection requirements: Plans for response to breach and HIPAA compliance measures.
- Termination clauses: Reasonable periods of notice and transitional support.
6. Negotiation Strategies
Refrain from the following areas during negotiations on contracts:
- Sanctions for underperformance: Impose financial penalties as sanctions on underperformance.
- Transition support: Provide suitable support on joining the service and any subsequent changes.
- Reporting obligations: Detail the reporting frequency and presentation.
- Audit rights: Maintain rights to audit billing process and accuracy.
7. Making Your Final Decision
Comprehensive Evaluation Framework
Use this systematic approach in the final selection:
- Weighted scoring: Use the same criteria on all the candidates with the following evaluation matrix.
- Reference checking: Call a minimum of 3-5 recent clients for in-depth performance reviews.
- Pilot testing: Try out actual performance on short-term test periods.
- Cost Analysis: Calculate the total cost of ownership along with any migration costs.
8. Implementation Planning
The leading medical billing company provides systematic implementation support:
- Development schedule: Specific dates for go-live and system integration.
- Employee education: Thorough training on new procedures and communication.
- Staff training: Comprehensive education on new processes and communication protocols.
- Monitoring performance: Simultaneous monitoring of key indicators in order to facilitate smooth handover.
- Ongoing support: Personal account handling and quarterly performance check-ins.
9. Future-Proofing Your Billing Partnership
Emerging Industry Trends
Stay one step ahead of market advancements by selecting partners prepared for:
- Value-based care models that require quality metric monitoring. Complexity in billing telehealth because of increasing remote care services. Improvement in patient financial experience through price transparency and variable payment.
- Incremental updates such as possible ICD-11 implementation and revised Medicare recommendations.
10. Long-Term Partnership Success
Create lasting relationships with:
- Scheduled review periods with data-based conversations regarding areas of growth.
- Statements on forthcoming industrial developments that impact your work.
- Technical advancements, keeping your billing process updated with new industry practices.
- Ongoing education brings your in-house team up-to-date on billing best practices.
Frequently Asked Questions:
Medical coding involves reviewing patient documents and assigning appropriate diagnosis and procedure codes. Medical billing takes those codes and processes claims to insurance companies for payment. While related, these are separate functions that require different expertise.
Look for companies that are properly certified (AAPC or AHIMA), A+ BBB ratings, HIPAA compliant forms, and additional client referrals. Companies like Human Medical Billing demonstrate credibility with 20+ years of experience, BBB membership, and transparent business practices.
Either can be excellent. National businesses have more money and technology, whereas local businesses have the ability to provide better service. Emphasize capability, indicators of performance, and distinctive expertise rather than location.
Standard reports consist of clean claim rates, denial rates, days in accounts receivable, collection rates, and aging reports. Reporting must be accomplished on at least a monthly basis, and key performance dashboards must include real-time access.
Improvements typically occur in 30-60 days, and complete optimization is always achieved in 90 days. Early benefits are typically lower denial levels and faster claims.
Conclusion: Your Roadmap to Billing Mastery:
Choosing the best medical billing company requires careful attention among a host of factors like specialty experience, technological know-how, price transparency, and performance guarantees. It impacts every aspect of your practice’s financial health, from cash flow and reimbursement all the way through compliance.
Organizations such as Human Medical Billing represent the best practices with A+ BBB accreditation, over 20 years of experience, month-to-month flexible contracts, and straightforward integration with 25+ EHR products. They offer personalized account management, and one-on-one service without any trade-offs on industry leading performance metrics.
The future medical billing environment will remain one of AI automation, value-based care demands, and elevated patient fiscal experience. Choosing a forward-looking partner who is ready for these changes is the key to long-term success for your practice.
Allow yourself time to thoroughly assess possible partners through the lenses offered by this guide. Your decision on a billing company will impact the financial health and growth path of your practice for decades to come. Make it meaningful.

