TL;DR: How to Cut After-Hours Charting (Fast)
To reduce EHR time for physicians, implement standardized note templates, include pre-visit planning, streamline the EHR inbox with shared pools and intelligent routing, and automate billing-related administrative tasks like prior authorizations and denial notices. Enhance these improvements with AI documentation tools. To confirm improvement, monitor pajama time, encounter closure, and inbox task metrics.
Why EHR Work Follows Doctors Home (The Data)
For years, health care has operated under a silent rule - the patient is always prioritized, even if it means the doctor has to sacrifice their personal life. In the digital age, “pajama time” has become the most striking illustration of that portion of life that has to be given up.
When the clinic doors shut, the work of the doctor is not done. Physicians still need to catch up with electronic health records in the evenings. Scribing, billing, replying to messages, and even manual prior authorization submissions are a handful of the tasks that dominate physician’s schedules, loaded with a mountain of sustained work that is inefficient and overly taxing.
Time in EHR per Visit & After Hours (Benchmarks)
The AMA 2025 physician survey reveals new findings:
- Physicians allocate 27.2 hours weekly in patient engagement.
- A further 13 hours in ancillary services like referrals and result evaluations.
- Approximately 7.3 hours weekly in strictly clerical roles such as filing insurance claims.
Entering the data, we hit a staggering 58 hours of work, the vast majority of which finishes well past the office clock-out time.
A recent JAMA Network Open study highlighted pajama time as ~6 minutes per physician visit. JAMA Network Open (2023). For 80-100 patient physician, this translates to 8 to 10 hours of work per week, that is heavily concentrated in the evenings.
Burnout Link: What Studies Show
What matters most? The fact that physician burnout is correlated with time spent on an EHR.
- In 2024, 43% of physicians reported at least one symptom of physician burnout.
- Physicians who spend more than 90 minutes on pajama time have their burnout risk increased by nearly two times.
- Burnout leads to an increase in medical errors, reduced patient satisfaction, and increased early attrition from the workforce.
- There is a substantial financial burden, a single physician can cost a hospital $250,000 to $500,000 in recruitment, onboarding, and lost productivity.
The connection is crystal clear; the workforce is qualitatively and quantitatively protected by reducing pajama time, which is more than just a matter of convenience.
The Human Toll of Pajama Time
Statistics are interesting, but real experiences are even more conclusive. Doctors often talk about what they do in the evenings: after putting the children to bed, they switch on their laptops to complete their forms.
In 2025, an internist said in the AMA News Wire: "I spend more time documenting why I provided care than providing care. By the time I finish, I'm too exhausted to spend time with my family."
This evening routine nibbles away at rest, family time, and resilience. It also sustains a sense of futility: if all the hours of charting are not clinically significant, the workload becomes demoralizing.
The cost in human lives emphasizes why pajama time reduction should be addressed as a system-level issue.
What Actually Works (Toolkit to Reduce EHR Time for Doctors)
There is no silver bullet that eliminates pajama time. But research indicates a stack of interventions that, collectively, produce a measurable effect.
Templates & Pre-Visit Planning
Standardized note templates facilitate easier repetitive documentation, reduce variability, and help in getting notes aligned with billing requirements.
Using templates with pre-visit planning where support staff have histories, lab reports, and forms ready before the visit makes post-meeting charting easier.
On AMA pilots, clinics utilizing both interventions experienced 20–25% reductions in chart completion time.
Inbox Protocols (Routing, Pools, Filters)
Patient portals and secure messaging were used to expand access but have instead become one of the fastest-rising causes of pajama time. Doctors now must contend with hundreds of messages in their inboxes each week.
Evidence-based inbox redesign includes:
- Shared pools to distribute messages across clinical teams.
- Routing protocols that direct admin questions to non-physician staff.
- Filters that prioritize urgent clinical items.
AMA’s Inbox Burden Toolkit shows practices that adopt pooling and routing reduce both pajama time and patient wait times for message responses.
Delegate Billing, Prior Auth, and Denials
Billing-related documentation may be the most underappreciated reason for pajama hour. Every diagnosis has to comply with coding rules; every prior authorization has to be documented thoroughly; every denial requires more work.
Most practices choose to do this by employing outside revenue cycle staff such as Human Medical Billing. Outsourcing tasks such as denial management, prior authorizations, credentialing, and coding reviews means that physicians don't have to invest hours explaining claims after office hours.
When billing workflows are integrated seamlessly, charting becomes lighter and revenue cycles more predictable.
Ambient AI & Documentation: Where It Helps and Where It Doesn’t
AI scribes are generating buzz, but their real-world impact is nuanced.
- Pros: reduce manual typing, capture patient dialogue, shorten note-writing.
- Cons: accuracy risks, PHI governance, need for physician validation.
A 2024 JAMA Network Open study linked higher satisfaction with EHR usability to lower burnout odds but emphasized that AI tools should complement, not replace, human judgment.
Best practice: pilot AI tools selectively - especially in high-documentation fields like primary care and OB/GYN - and monitor outcomes closely.
Implementation Roadmap (30/60/90 Days)
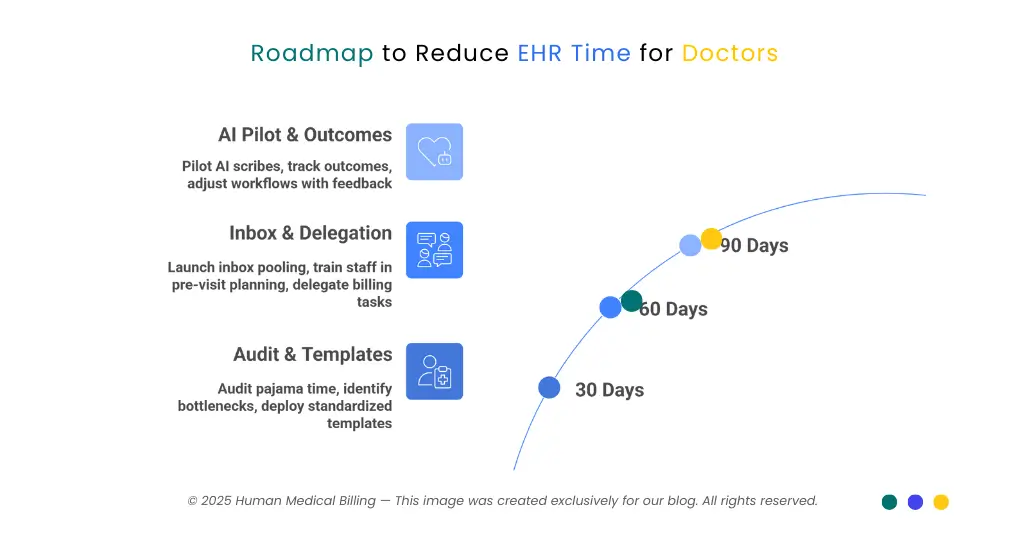
30 Days
- Audit pajama time using EHR logs.
- Identify top denial drivers and prior-auth bottlenecks.
- Deploy standardized templates for common visits.
60 Days
- Launch inbox pooling and routing protocols.
- Train staff in pre-visit planning workflows.
- Delegate denials and prior-auths to RCM partners.
90 Days
- Pilot AI scribes in targeted specialties.
- Track outcomes: pajama time minutes, inbox volume, encounter closure speed.
- Adjust workflows with physician feedback and billing support.
By spreading interventions across 90 days, practices can demonstrate quick wins without overwhelming staff.
Real-World Examples: Cutting Pajama Time
A primary care group in the Midwest piloted inbox pooling and outsourced prior authorization support to an RCM partner.
Results after 90 days:
- Pajama time fell 38%.
- Average encounter closure improved from 2.4 → 1.6 days.
- Denial rates dropped 15%, improving revenue stability.
An OB/GYN practice that standardized templates and introduced pre-visit planning saw a 30% reduction in note completion time within two months.
These examples confirm what research predicts: combining workflow fixes with billing offload produces measurable, sustainable relief.
| Metric | Benchmark (AMA/JAMA) |
|---|---|
| Pajama time per visit | ~6 minutes (JAMA Network) |
| After-hours charting threshold | ≤5 hrs/week = lower burnout odds |
| Physicians logging >8 hrs/week | 22% (AMA) |
| Burnout prevalence (2024) | 43% (AMA) |
| Cost of replacing 1 physician | $250K–$500K (PubMed) |
FAQ: Reducing EHR Time and Physician Burnout
It’s after-hours EHR work-notes, orders, inbox tasks - completed at home (PMC).
Around 6 minutes per visit; many log 6-8+ hours weekly (JAMA Network, AMA).
Yes. ≤5 hrs/week is associated with ~2x lower burnout odds (PubMed).
Templates, pre-visit planning, inbox protocols, billing offload, selective AI scribes (AMA Ed Hub, JAMA Network).
After-hours minutes, encounter closure, inbox load, denial rates, prior-auth turnaround.
Yes-positively. It reduces denials, prevents rework, and ensures coding compliance.
Yes. Risks include transcription errors and PHI security. Physician oversight is essential (JAMA Network).
Primary care, OB/GYN, internal medicine, and practices without internal RCM scale (AMA).
Conclusion: Reclaiming Time, Restoring Joy
Doctor’s ought to finish their days with families, not computers. Pajama time detracts from well-being, patient safety, and healthcare economics.
The answers are straightforward: implement workflow enhancements (templates, pre-visit prep, inbox protocols), outsource billing and denials to proven vendors such as Human Medical Billing, and pilot focused AI tools.
At Human Medical Billing, we have witnessed how these tactics save time, bring balance, and stabilize money flow. By addressing the top causes of pajama time, practices can keep doctors happier and enhance patient care as well.
To learn more, visit About Us, read Success Stories, view How Our Services Work, or peruse the Xpert Billing Blog.

