The medical industry is experiencing a revolution in 2025 and at the heart of this revolution is AI medical billing. Hospitals, clinics, and private practices are struggling to keep up with compliance, staff, and complex payer regulations, and therefore automation of healthcare billing is no longer an option but a necessity.
As stated by the American Medical Association (AMA), administrative expenses in the form of claim denials, manual coding errors, and delayed reimbursement translate into billions of dollars annually for healthcare providers. With the advent of medical coding AI and process automation, a revolution in the revenue cycle in the form of accuracy, efficiency, and transparency is being witnessed.
Here, we will detail how AI and automation are transforming medical billing in 2025, and what benefits they can offer to healthcare providers.
Why Medical Billing Needed a Revolution
Medical billing was for many years a highly manual, paper-based process. Billers and coders had to dig through patient files, assign ICD-10 codes, and send in claims to payers. Some of the typical problems were:
- Elevated claim denial rates due to mistakes of manual coding.
- Absence of standardization between payers.
- Personnel shortages because trained coders became harder to find.
- Addition of regulatory burden through regulatory reforms.
- Delayed payments and cash shortfalls for healthcare providers.
Healthcare Financial Management Association (HFMA) released a 2024 report that uncovered that claim denials have risen by 11% during the past three years, affecting the sustainability of the hospital revenue cycle. Providers began to seek healthcare billing automation as the next frontier.
The Rise of AI and Automation in Healthcare Billing
From robotic process automation (RPA) to machine learning algorithms, technological advancement has envisioned the future of revenue cycle management (RCM) differently. Some of the key drivers for this change are as follows:
1. Medical Coding AI
- AI programs today read electronic health records (EHRs), read reports, and assign correct ICD-10 and CPT codes in real time.
- This prevents coding mistakes, increases billing precision, and encourages compliance.
- Coding with AI decreases error rates by as much as 70%, as stated by AHIMA (American Health Information Management Association).
2. Claims Automation
- Automated AI-driven bots transmit clean claims electronically, signaling potential denials before submission.
- Natural language processing (NLP) helps identify discrepancies in clinical documentation.
3. Predictive Denial Management
- AI models are able to forecast denial patterns by some payers and auto-correct doc mistakes before submission through predictive analytics.
- Providers who embrace such Denial Management Services receive reimbursement earlier.
4. Patient Payment Automation
- Consumers are given AI-generated cost estimates and automatic billing reminders.
- This increases patient satisfaction and reduces outstanding Medical Accounts Receivable Services.
Benefits of AI Medical Billing in 2025
Let’s look at how AI medical billing is helping physicians, practices, and health systems thrive in today’s landscape:
| Challenge | Traditional Billing | With AI & Automation |
|---|---|---|
| Coding Errors | Manual and prone to mistakes | Medical Coding AI ensures 70–90% accuracy |
| Claim Denials | Average rate of 10–12% | Predictive denial management reduces to <5% |
| Payment Delays | 30–60 days on average | Automated RCM reduces cycle time significantly |
| Staff Burden | High reliance on billers/coders | AI supports staff, reduces burnout |
| Compliance Risks | Frequent regulatory misses | AI updates rules in real-time |
Automation has turned billing from reactive to proactive. Rather than waiting for a denial, providers can avoid claims from being denied at all.
Becker's Hospital Review (2025)
Applications Across Revenue Cycle
AI and automation enhance not just one but multiple stages of the healthcare revenue cycle:
- Eligibility Verification – AI verifies insurance eligibility in real time.
- Medical Coding Services – Computerized ICD-10, CPT, HCPCS coding.
- Charge Capture – Identifies outstanding charges in documents.
- Claim Scrubbing – Auto-corrects claims before submission.
- Denial Management Services – Predicts, prevents, and appeals claims more effectively.
- Medical Accounts Receivable Services – Automates payment processing, patient reminders, and follow-ups.
- Analytics and Reporting – Provides practice managers with actionable information.
The Human Touch: Why AI Doesn’t Replace but Enhances
One of the biggest questions that most medical professionals ask is: Will AI replace billers and coders?
The response is no. But it does make their work better. The AAPC (American Academy of Professional Coders) determines that AI is an enabler - accelerating routine tasks, decreasing repetitive work, and enabling coders to handle complicated cases that involve clinical judgment.
At Human Medical Billing, we believe that by combining the best-of-breed AI medical billing technology with human perspective, we achieve accuracy, compliance, and the empathy that automation by itself cannot.
Key Industry Trends in 2025
Below are some trends which alter the landscape:
- Value-Based Care Integration: AI facilitates the integration of the new payment models through associating billing with outcome.
- EHR Interoperability: Smooth integration guarantees coding consistency among systems.
- AI-Driven Compliance Monitoring: HIPAA and payer regulation real-time alerts.
- Voice-Enabled Coding: Physicians talk and AI codes them instantly.
- Blockchain in RCM: Increases data security and transparency.
Practical Guide: How Providers Can Adopt AI Medical Billing in 2025
Implementing AI medical billing is daunting to physicians. With compliance mandates of payers, and cost, it is no wonder that most clinics are reluctant to take the plunge. Yet, with a well-designed approach, automation is simple to integrate into current procedures without disrupting care to patients.
Here is a real guide to providers considering AI billing this year:
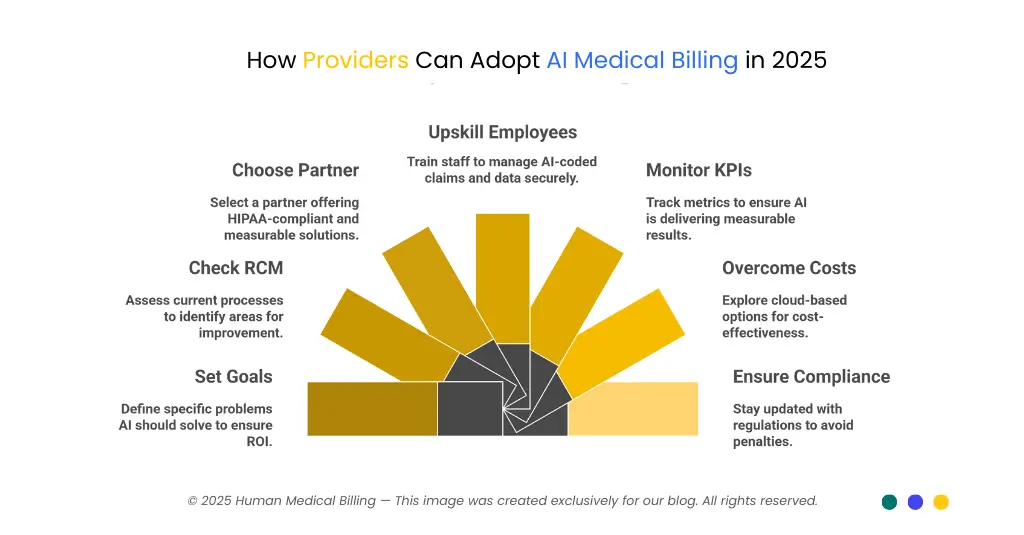
1. Set the Goals:
- Start by breaking up what problems you'd want AI to solve
- Are denials a chronic issue? Is your current Medical Accounts Receivable Service slow?
- Do you not have enough coders to achieve accuracy?
With well-defined goals in mind, the technology you're introducing to the market is generating staggering ROI rather than just offering another gadget.
2. Check Your Current RCM Installation
Before you invest in automation, walk through your Healthcare Revenue Cycle Management Services process:
- What's your denial rate for today?
- Average payment posting time?
- Cash flow deficits?
Industry guidelines (from HFMA, 2024) state that a clean claims rate of over 95% is optimal. If your practice is far lower than that, AI is the potential game-changer.
3. Choose the Right AI Partner
Not all solutions are equal. Look for medical billing partners who:
- Provide Medical Coding Services that involve AI.
- Use HIPAA-compliant platforms.
- Offer clear performance measures.
At Human Medical Billing, we couple automation with experienced Medical Billing Services, so that providers do not have to make a choice between efficiency and compliance.
4. Upskill and Train Employees
AI never replaces coders, it makes them better. Offer billers and coders training in:
- Auditing AI-coded claims.
- Managing exceptions generated by automation.
- Handling confidential patient data safely.
Practices that invested in staff-AI collaboration, as per the AAPC (2025), had denial rates reduced by a mean of 18% compared to practices that utilized automation without monitoring.
5. Monitor KPIs post-implementation:
- More than 90-day denial rates
- Cost per claim
- Patient billing satisfaction scores
They inform you whether your utilization of AI is generating measurable results.
6. Overcome Cost Challenges
Most of the small practices believe AI implementation is too expensive. Cloud-hosted AI billing systems are billed per-claim or per-provider, so it is viable even for single practices. In the long term, faster payments eventually pay back the initial cost.
7. Ensure Secure and Compliant:
AI needs to be regularly updated with CMS guidelines, payment policies, and HIPAA data security norms. Reliable vendors like Human Medical Billing stay current with the new regulations, thereby avoiding providers from facing penalties.
Why This Matters in 2025
In today's health environment, automation healthcare solutions are not an option. Those who delay risk falling behind in cash flow, patient satisfaction, and compliance. Those who adopt AI early, however, lock in their financial well-being and buy time to improve patient outcomes.
By taking this route, all practice - small or large - can utilize the potential of AI medical billing successfully in 2025.
Future Outlook: Where AI Medical Billing Is Headed
Looking forward:
- 100% automated claims cycle: From coding to payment posting with little human input.
- More transparent patient bills: AI will segment costs into patient-friendly presentations.
- Adaptive learning: Artificial intelligence invoicing systems will correct themselves automatically according to payer feedback.
- Global uptake: Other countries beyond the U.S. will utilize the same models with standardization.
The future is bright: AI physician billing and computerized healthcare systems are no longer an option - they are the way to stay competitive and financially stable in 2025 and later.
Conclusion
With medical costs on the rise and compliance more complicated, practices that embrace AI medical billing and healthcare automation will be ahead of the game. AI and automation not only improve billing accuracy but also allow providers to return to doing what they do best - healing patients.
We at Human Medical Billing specialize in matching healthcare providers with cutting-edge Healthcare Revenue Cycle Management Services. Our offerings combine:
Artificial Intelligence-driven Medical Billing Services that reduce errors and speed up payments.
- Denial Management Services to keep revenue intact.
- Medical Credentialing Services to prevent delays in reimbursement.
- Medical Coding Services with added automation.
- Medical Accounts Receivable Services accelerating collections, reducing collection cycles.
Want to know how AI can transform your billing processes? Contact us today to find out more about our commitment to healthcare practice.

