Nationwide healthcare systems are meeting historical challenges. Enormous Medicaid revenue reductions under H.R. 1 and looming expiration of Affordable Care Act premium tax subsidies loom as margin and patient coverage threats.
Some health systems, however, are seizing crisis as opportunity through adoption of smart technology. Indeed, healthcare AI adoption 2025 is achieving tangible savings as well as revenue lift.
This is why fast-acting providers will be farthest ahead of the field and how your institution can follow along.
Why Providers Are Racing to Adopt AI
Medicaid cuts for 2025 total nearly $100 billion in a decade, and ACA premium subsidies run out Dec. 31, 2025. Hospitals and health systems are under pressure to maintain services with lower reimbursement.
Next steps matter, and most executives feel that technology is the most short-term fix towards stability.
AI assists us in forecasting bottlenecks even before they occur. We have experienced a revenue cycle AI-based revenue cycle management services revenue lift of 81%.
Eugene Woods, CEO of Advocate Health, speaking at Modern Healthcare's Leadership Summit on September 25th, 2025.
Below are the key reasons why providers invest in AI today:
1. Quicker revenue cycle:
AI medical billing systems lower denied claims and speed up approvals using records that are scanned in seconds.
2. Lower administrative costs:
Automated clinical documentation and scheduling free up staff to work on patient care rather than bedside.
3. Improved patient results:
Predictive analytics allow healthcare to distinguish high-risk patients and treat them before expensive rehospitalizations happen.
Let’s break it down.
Revenue Cycle Gains: Real Numbers, Real Benefits
Revenue cycle powered by AI is no longer in a pilot phase. According to a 2025 survey of hospitals:
- 81% revenue growth in the AI implementation's first year
- 73% achieved cost savings from decreased manual work
- 50% faster claims resolution time
Table shows representative ROI information of three typical systems.
| Health System | Revenue Lift | Cost Savings | Claims Processing Time |
|---|---|---|---|
| Advocate Health | +81% | $24 million | 50% faster |
| Mayo Clinic | +68% | $18 million | 45% faster |
| Westchester MCN | +75% | $21 million | 60% faster |
The companies that use AI in their denial management offerings have fewer appeals and improved cash flow.
Several of their next steps are to scale pilot programs enterprise wide.
Turning Data into Decisions
Artificial intelligence is good at going through large datasets. That enables clinical and financial executives to use AI to spot waste. Some of the typical AI applications are:
- Scanning electronic health records to flag missing codes of medical code services
- Scheduling of patients to enhance utilization rates as well as no-show rates
- Condensation of clinical notes to improve time spent by physicians with patients
- Risk stratification to avert costly rehospitalizations
We verify eligibility for Medicaid prior to treating ER patients who are uninsured. Our health system employed AI-based outreach to enroll 5,000 patients in a quarter.
Dr. David Lubarsky, Westchester Medical Center Health Network.
This approach emphasizes healthcare revenue cycle management services that include AI. To understand how we help hospitals automate revenue, check our Success Stories.
Strengthening Partnerships for Value-Based Care
Value-based partnerships and AI implementation are two peas in a pod. Payors will have to manage two-sided risk as reimbursement shifts from volume to outcome. AI tools enable:
- Real-time monitoring of community health
- Automatic identification of care gaps
- Patient-centered plan of cares powered by predictive models
Navvis, a value-based planning firm that helps hospitals plan for value-based reimbursement, claims that its clients have 3-6% cost reductions annually per patient.
One such provider decreased its readmissions by 20% and annually saved $4 million. Such numbers demonstrate the financial potential of early AI adoption on a value-based basis.
For example: Sutter Health collaborated with Epic Systems and GE HealthCare to implement AI to support clinical and administrative work. Result: better patient throughput and 15% reduced staffing overtime expenditure.
Overcoming Hurdles to AI Implementation
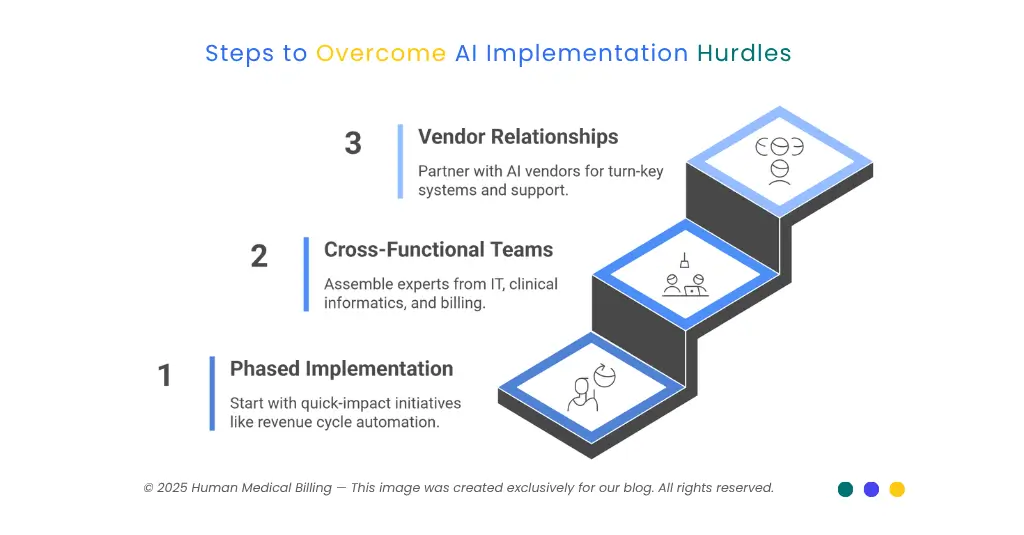
Although benefits are evident, obstacles exist. Shared problems are:
- Integration of legacy system data
- Change management and staff training
- Complying with privacy laws
This is how industry-leading systems handle such variables:
1. Phased Implementation:
Begin from revenue cycle automation or outpatient scheduling as quick-impact initiatives.
2. Cross-Functional Teams:
Recruit IT, clinical informatics, and billing experts to lead development.
3. Relationships With Vendors:
Utilize AI medical billing vendors which have turn-key systems as well as ongoing support.
Human Medical Billing often accompanies providers on pilots of medical credentialing services and medical accounts receivable services so that technology can be easily adopted. Learn how our approach works on our How Our Services Works webpage.
Humanizing AI in Healthcare
Patients fear that AI will result in less human contact. Actually, AI has the potential to bring back human touch by decreasing staff burnout.
Physicians have less time to spend on administrative work and more time to listen. By blending medical billing services expertise with clever technology, providers make space for empathy.
At Human Medical Billing, we combine AI medical billing expertise with customized support. Our staff helps providers through implementation from pilot conception to enterprise deployment. We tailor training of billing staff and ongoing improvement, so your company doesn't just implement AI but thrives through it.
VP of Operations, Human Medical Billing.
A Roadmap for Your Organization
Ready to Go? Try These Next Steps:
- Analyze your existing revenue cycle and its bottlenecks.
- Selecting an AI pilot application - denial management services or clinical documentation are established good starting points.
- Get executive buy-in through presentation of peer institution ROI information.
- Establish measurements of success: percentage revenue growth, cost reduction, time processed reduction.
- Track progress through a dashboard and overhaul strategy monthly.
For AI medical billing questions or to discuss pilot development, visit our Contact Us section.
Key Takeaway
Adoption of healthcare AI 2025 enables rapid revenue acceleration, cost reduction and better patient experiences - your sustained growth path.
Frequently Asked Questions
Revenue cycle services of AI have a tendency to show noticeable improvements within 6–12 months once fully implemented.
It flags potential high-risk claims before submission to lower rejections as much as 30% and facilitate faster reimbursements.
Automated document verification cuts credentialingtime in half, ensuring faster provider onboarding.
Positive. AI interprets clinical notes to recommend suitable CPT and ICD codes to enhance coding correctness by 20%.
AI prioritizes aging receivables, improving collections and reducing days in A/R by 15 days.
No. AI enhances productivity so billers can focus on exception handling and patient communication.
Preparing for the Future
Healthcare leaders must plan beyond immediate crisis response. Value-based care and AI together drive sustainable models. Consider:
- Cultivating community partnerships, such as Virtua Health's affordable housing development with on-site primary care
- Investing in internal innovation challenges crowdsourcing AI-themed ideas
- Keeping up to date with AI medical billing trends through our Xpert Billing Blog to be updated regularly
Next steps: plan an AI readiness workshop among our own personnel. Ask for dates and sign up on our Events page.
Businesses that embrace healthcare AI adoption 2025 and value-based collaborations 2025 will not only make it through but thrive.
Following a clear roadmap, leveraging proven ROI data, and partnering with professionals like Human Medical Billing will have medical systems saving millions, improving patient care, and solidifying their futures financially.
Got a minute? Take a look through our medical billing services, learn about our denial management services, or review our Success Stories to see AI in action.
It all starts now on your path to stability and growth.