Medicare's traditional fee-for-service (FFS) program pays billions of dollars worth of medical claims annually, but much of that payment crosses over to finance wasteful or unneeded medical care. To combat such inefficiencies and stem spiraling costs, the Centers for Medicare and Medicaid Services (CMS) launched the innovative Wasteful and Inappropriate Services Reduction Model (WISeR) in July 2025. This is a new pilot program utilizing artificial intelligence (AI) to apply prior authorization (PA) more aggressively at reduced cost to Medicare.
As a pilot for six years, the CMS WISeR model is intended to reduce wasteful Medicare expenditure by more appropriately approving and rejecting claims. The pilot is initiated in six states - Arizona, New Jersey, Ohio, Oklahoma, Texas, and Washington - where private companies dispatch AI-driven prior authorization tools to rigorously examine medical claims.
This article explores the whole CMS WISeR model, analyzing its importance, operations, and impact on patients, doctors, and the future of Medicare billing in 2025.
What Is Prior Authorization in Medicare?
Prior authorization is a widely used utilization management process where healthcare providers must obtain approval from Medicare before delivering certain medical services or purchasing specific products. The aim is to ensure that recommended care is medically necessary and clinically appropriate prior to services being provided and reimbursed.
In Medicare Advantage and most private insurance, prior authorization has been standard practice for decades. But in fee-for-service (FFS) traditional Medicare, it was not employed as frequently in the past. Legal mandates and the open-network philosophy of the program, whereby all qualified providers are reimbursed, meant fewer prior authorization requests.
In the last few years, CMS has introduced prior authorization programs for Medicare FFS. For example, the 2022 pilot, which imposed PA on orthoses (surgical braces), demonstrated enormous cost savings. Orthoses expenditures dropped dramatically from $33.5 million Q1 2022 to as low as $8.8 million Q3 2023, demonstrating how PA reduces waste.
The CMS WISeR Model: AI Meets Prior Authorization
The CMS WISeR model is a move in the right direction. It is piloting a six-year program employing detailed prior approval for 17 high-risk, specific services. The model employs sophisticated AI technology and machine learning to review and approve claims before medical services are provided.
CMS collaborates with seasoned private firms in prior authorization, a number of which have commercial insurance industry experience, to handle such screenings. The firms employ sophisticated AI software to rapidly and accurately scan clinical documents, medical necessity guidelines, and history to determine whether claims qualify.
Exclusive only to WISeR, these contractors are paid fee-for-savings for rejecting inappropriate claims, incentivizing proper and prompt screening rather than batching denials or delays.
The model has been operational since summer 2025 and now operates in six states: Arizona, New Jersey, Ohio, Oklahoma, Texas, and Washington. The demonstration is split into two phases spanning three years each and CMS is monitoring how it goes. They monitor things such as costing savings, patient outcomes, and provider feedback.
Why the CMS WISeR Model Matters: Fighting Wasteful Medicare Spending
More than 1.1 billion Medicare FFS claims were paid in 2021. Wasteful and avoidable spending is the biggest risk to the program's future. Experts say billions of dollars can be saved annually by not performing unnecessary medical procedures.
The Government Accountability Office (GAO) supports prior authorization policies used by the government responsibly to limit wasteful expenditures at the expense of maintaining essential patient access. The success of CMS's prior orthoses PA pilot provides initial evidence that concentrated efforts can limit wastefulness without injuring beneficiaries.
The WISeR demonstration model for CMS is quite crucial as it employs existing AI technology to assist with Medicare billing administration. This assists in more accurately identifying suspicious claims by bringing together clinical guidelines, provider history, and data analysis—much more than the previous manual review process.
Addressing Political and Provider Concerns Around WISeR
The WISeR model at CMS has experienced political as well as practical issues despite the fact that it is full of potential. Forty House Democrats sent a letter to CMS advising them not to give contracts to for-profit prior authorization firms. They are concerned that these firms will deny healthcare too aggressively, which will restrict patients' access to it.
Pilot state providers are concerned about increased administrative burdens and potential treatment delays. Providers are concerned that the increased paperwork and waiting time PA will involve will impair their work flow and patient satisfaction.
CMS is aware of these issues and has promised to review the program extensively. They can end the demonstration if they find adverse effects, including higher denial rates or harm to patients.
AI decision-making needs to be transparent, and CMS is attempting to make the decision-making technology credible and understandable to healthcare providers.
What the CMS WISeR Model Means for Providers and Patients
WISeR pilot state providers must comply with new prior authorization requirements that demand robust clinical documents prior to service approval. This is more involved, but leveraging AI decision support can make workflows easier and decisions faster.
For beneficiaries, the aim is to save Medicare dollars by ending wasteful treatment without compromising timely access to needed treatment. CMS will continue to monitor patient experiences and outcomes to ensure that the model does not compromise access to care.
Since needs are evolving, it is highly essential to work with professional medical billing firms such as Human Medical Billing. Employing their expertise in Healthcare Revenue Cycle Management Services, Medical Coding Services, and Denial Management Services, Human Medical Billing assists providers in complying with prior authorization regulations with ease and recovering maximum money.
The Role of AI in the Future of Medicare Billing
WISeR demonstrates the ways artificial intelligence is transforming healthcare management. AI systems assist in automating routine claim checks, locating fraud or billing errors, and forecasting unnecessary or dangerous treatments, which enhances the way things function.
Healthcare professionals should be working with billing partners who utilize AI technology. These partners offer services such as AI Medical Billing and Medical Accounts Receivable Services. They assist in enhancing revenue cycles, reducing denial rates, and keeping pace with rapid digital evolution.
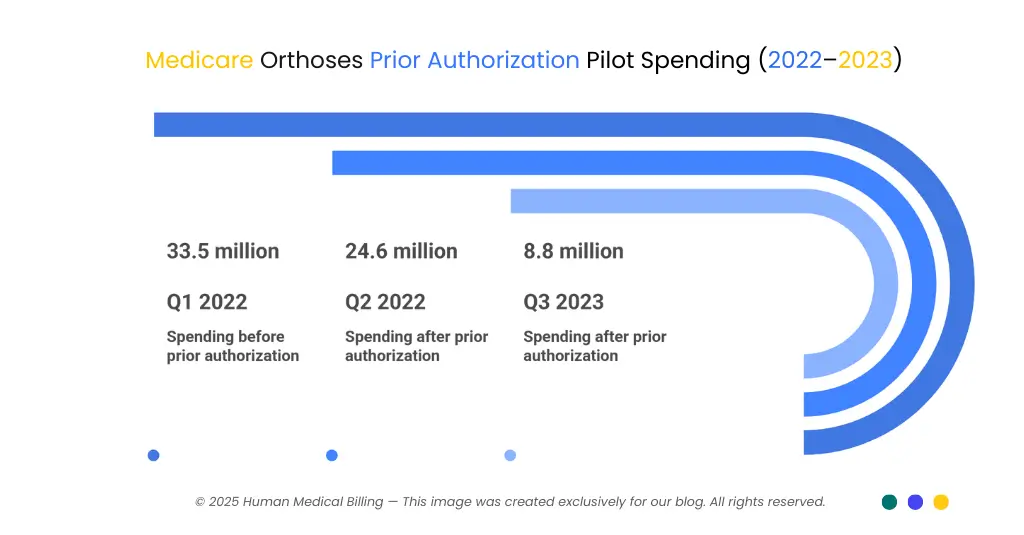
| Quarter | Medicare Spending (USD Millions) |
|---|---|
| Q1 2022 (pre-PA) | 33.5 |
| Q2 2022 | 24.6 |
| Q3 2023 | 8.8 |
Frequently Asked Questions About the CMS WISeR Model
The WISeR model is a six-year Medicare demonstration that applies AI-powered prior authorization to reduce waste in the traditional fee-for-service Medicare program.
CMS officially announced and began the WISeR demonstration in July 2025.
Arizona, New Jersey, Ohio, Oklahoma, Texas, and Washington.
By ensuring only medically necessary services are approved, prior authorization reduces overuse and the resulting wasteful spending.
CMS is closely monitoring this risk and aims to balance more precise denials with timely access to necessary treatments.
Final Thoughts
The CMS WISeR model is a major move toward more efficient Medicare spending control through the aid of AI. It is currently in the experimental phase, but early results from comparable initiatives suggest that it can potentially save billions of tax dollars without jeopardizing care quality.
Healthcare providers in affected states must prepare by working together with seasoned billing firms such as Human Medical Billing. They provide full Medical Billing Services and cutting-edge AI Medical Billing services that are intended to address the issues of prior authorization.
Stay current with Medicare policy changes and enhance your revenue cycle management today by checking out our Xpert Billing Blog, and FAQs.

