What is the CMS LCDS Version 5.1 Update for 2026?
CMS issued a critical errata on December 5, 2025; which was an update to the LCDS Manual Version 5.1, effective January 1, 2026. The update made changes to the coding definitions of item J1900 (Falls with Major Injury) by specifying that all traumatic injuries including joint dislocations, internal organ damage and crush injuries are considered major injuries. The failure to adhere to such definitions may adversely affect a facility's ability to report accurate data in regard to the Long-Term Care Hospital Quality Reporting Program (LTCH QRP); thereby impacting the facility's Annual Payment Update (APU).
Introduction: The Clock is Ticking for LTCH Compliance
The regulatory environment for long-term care hospitals (LTCH) has changed yet again. Many providers have not had time to absorb last fall’s changes to the fiscal year updates since they were made in October and now CMS has implemented a mandatory, mid-year update that all LTCH must immediately comply with.
CMS on December 5th, 2025 released an Errata Document that modified the LCDS manual version 5.1. The Errata document is NOT optional - it is a requirement. As of January 1st, 2026, the definitions for patient falls and injuries (specifically items J1750, J1800 and J1900) are changing.
These changes require immediate action by hospital administration and Health Information Directors (HIDs), as these changes impact the LTCH QRP (Quality Reporting Program) results for your hospital. Your coding staff cannot continue to utilize the 2025 definitions after January 1st, 2026 or your reporting will be incorrect. Healthcare Compliance professionals know that inaccurate reporting can create operational risks.
Human Medical Billing understands that complying with CMS mid-year correction changes is a task that no one wants to do - however the injury coding changes to the injury codes are important to protect your hospital’s reputation and to maintain the integrity of your revenue.
Below is a summary of what is being changed; why it is important; and how you need to prepare your team for the new requirements.
The Core Update: J1900 and the New Definition of "Major Injury"
The most important part of the changes in this Errata is J1900 - Number of Falls Since Admission.
There was a long-standing ambiguity between the terms 'major' injury vs. 'standard' injury. The new CMS guidance eliminates this ambiguity. The definition for a 'major' injury will now be broadened to include additional types of traumatic events and will be more inclusive.
What Counts as a Major Injury in 2026?
In the past, coders would typically limit the term 'major injury' to broken bones or closed head injuries. The revised LCDS version 5.1 Errata includes the following conditions as examples of major injuries:
- Traumatic Bone Fractures: Excluding pathological fractures that occur due to disease i.e., Osteoporosis
- Joint Dislocations & Subluxations: Must be included in J1900
- Internal Organ Injuries: Any trauma to an internal organ
- Amputations: Trauma causing amputation of a limb due to a fall
- Spinal Cord Injuries: Any trauma to the spinal cord
- Head Injuries: Including head injuries that result in an altered level of consciousness or subdural hematoma
- Crush Injuries: Specifically clarified to require meticulous documentation
Importance of Accurate Documentation
Clinical documentation improvement (CDI) is critical to ensure the accuracy of your medical coding services. For example, if a nurse documents that the patient "fell and dislocated their shoulder", yet the coder did not document the dislocation as a 'Major Injury' per the revised J1900 rules, your data submission may be inaccurate.
Additionally, the update to item J1800 (Any Falls Since Admission) and item J1750 creates a ripple effect throughout your entire assessment process. The clinical staff need to provide more detailed documentation of the nature of the injury than they have in the past. Simply documenting "the patient complained of pain after falling" is no longer acceptable; the type of trauma needs to be identified in order to determine if the injury qualifies as a 'Major Injury'.
The Financial Stakes: Protecting Your Revenue Cycle
Why does CMS care so much about what you code as a fall? That will be explained through the LTCH Quality Reporting Program (QRP).
Data submitted to the LCDS for the purpose of calculating quality measures (specifically the Falls with Major Injury FMI measure), will be reported publicly on the Care Compare website. Patients and their families will view this site when determining which long-term care hospital provides the safest environment.
The Annual Payment Update (APU) Risk
Although a 2% decrease in your Annual Payment Update (APU) is based on not meeting data completeness thresholds (i.e., reporting at least 85% of all assessments); continuous coding inaccuracies may also undermine your facility's ability to achieve valid thresholds. Therefore, if your facility continually has data rejected or deemed invalid due to errors in the J1900 coding of falls, there is a high risk of having your facility fail to meet the required compliance threshold.
Therefore, a 2% decrease in Medicare reimbursement is an unacceptable risk to a busy LTCH. As such, the accuracy of your healthcare revenue cycle management services is critical. Your company is not only responsible for generating accurate claims but also for providing quality data to support those claims.
Human Medical Billing emphasizes that your revenue cycle begins upon patient admission. An inaccurate or incomplete LCDS assessment at the beginning of the patient's stay undermines the financial health of the organization prior to the claim being generated.
Looking Ahead: The Draft LCDS Version 5.3 (October 2026)
In addition to the January, 2026 deadline for the J1900 update, CMS has issued an outline of the proposed version 5.3 of the Long-term Care Data Set (LCDS), which is expected to be implemented as of October 1st, 2026.
Version 5.3 indicates a substantial shift from focusing on clinical-based outcomes, towards assessing the impact of the social determinants of health (SDOH) and collecting data on those social conditions that can affect the patient's ability to recover.
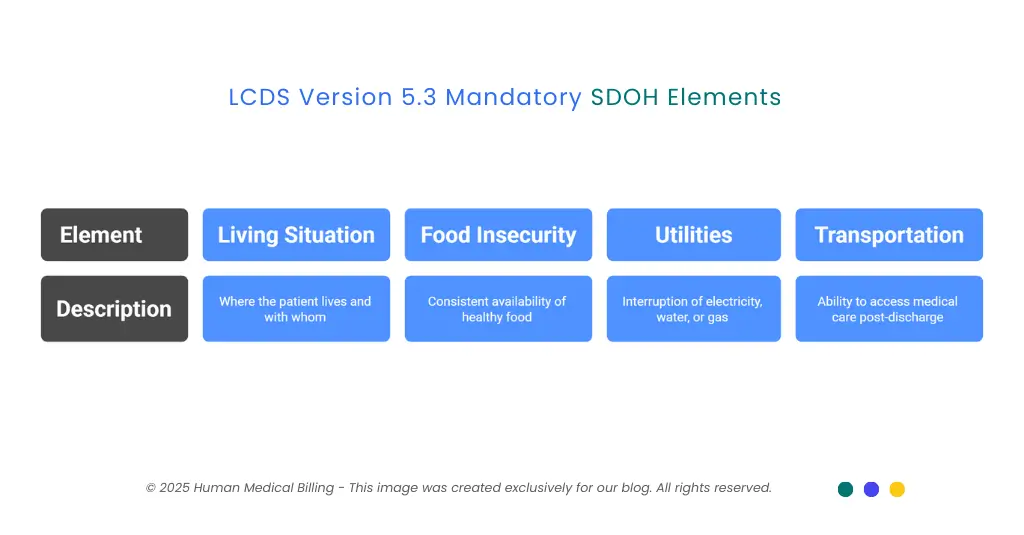
New Mandatory SDOH Collection Elements to Collect
Proposed by the draft of version 5.3 are four mandatory elements of data to be collected from patients at the time of admission; specifically:
- 1. Living Situation:
Where the patient lives and who they live with. - 2. Food Insecurity:
Is there consistent availability to the patient of healthy food? - 3. Utilities:
Did the patient go without electricity, water or gas within the last twelve months? - 4. Transportation:
(Modified) Will the patient be able to get to their medical care after being discharged?
These represent a major paradigmatic change to the admissions process. Your admissions personnel will require instruction as to how to inquire about these personal and often sensitive issues, in a way that is both compassionate and accurate.
Preparation for version 5.3 now will allow you to avoid the panic and scramble anticipated for Q3 of 2026. This is another example of why it is advantageous to engage in forward thinking medical credentialing services and to train your staff to be compliant with emerging regulations.
Strategic Action Plan: How to Ensure Compliance
With the 1st of January 2026 fast-approaching, and the transition of your facility to the updated LCDS Version 5.1 in full swing, we advise you to follow the recommended four steps below to assist you in achieving an efficient and smooth transition to the updated version of the LCDS Version 5.1.
1. Step #1. Review/Update Your Existing Fall Incident Reports (Documentation)
Review all your existing fall incident reports. Is the nurse clearly documenting dislocations or crush injuries within their report? If the report only documents a fall with injury, the coder(s) will not have the necessary information to document the required J1900 elements to meet the updated coding requirements.
2. Step #2. Update Your Coding Processes/Work Flows
Your Health Information Management (HIM) department needs to review the CMS Errata immediately.
- Action #1: Review the CMS Errata on the CMS website
- Action #2: Review/update your internal coding "cheat sheets" to include the updated list of Major Injuries (Subluxation, Internal Organ Injury, etc.)
- Action #3: Verify that your coding software has been updated. If you are using AI-based medical billing tools, verify that the algorithms have been revised to indicate the identified specific injury types.
3. Step #3. Provide Clinical Training for Your Clinical Staff
As previously mentioned, coding is only as accurate as the documented information provided by the clinical staff. We suggest conducting a short in-service training for your nursing and therapy staff explaining the difference between pathological fractures (osteoporotic related) and traumatic fractures. It is critical to provide this education as the clinical staff's documentation will significantly affect the accuracy of your organization's data reporting.
4. Step #4. Partner with Compliance Experts
If your internal compliance team is feeling overwhelmed by the constant flow of Errata and manual updates, it may be beneficial to seek assistance from an external compliance professional.
Human Medical Billing has over 20+ years of experience providing compliance support to healthcare organizations. While we specialize in processing claims, our company also acts as a compliance safety net. Whether you require denial management services to recoup lost revenue or a medical accounts receivable audit to improve the integrity of your organization's financial records, we can help.
Frequently Asked Questions (FAQ)
The revisions defined in the LCDS Version 5.1 Erratum document become effective on January 1st, 2026. Therefore, all assessments with a target date on or after this date will need to follow the new guidelines.
No. CMS states that pathological fractures (fractures resulting from bone disease), are not considered major injuries for this specific item. Only traumatic fractures should be recorded as such.
Although the above-mentioned J1900 definitions relate to a Quality Reporting Measure, failing to properly report your data may result in a 2% loss in your Annual Payment Update (APU) as part of the LTCH QRP if your data is not reported at a level of at least 85%.
Yes. While we service individual private practice physicians, we also provide medical coding services and revenue cycle support that may extend beyond basic requirements to meet the needs of a hospital’s facility based requirements. Our goal is to make sure that your data accurately represents what you expect in terms of financial success.
Conclusion
A "Falls with Major Injury" change is one of the most obvious examples of how a small regulatory change may greatly affect an organization's operations. The new regulation changes the definition of "major injury," and therefore raises the bar for data detail that facilities will be required to report.
Don't let the Falls with Major Injury update sneak up on your organization. Today is the day to review the LCDS Version 5.1 Errata, Train Your Team and verify that your reporting is error free prior to the January 1 deadline.
Are you looking for a Revenue Cycle Partner to assist in streamlining your revenue cycle while keeping you compliant with changing regulations? Human Medical Billing provides the resources you need to allow you to focus on patient care through Medical Credentialing Services as well as Advanced Medical Billing Solutions.
What's Next? Is your facility prepared for 2026? Contact Human Medical Billing today for a complimentary consultation on your revenue cycle health. We want to help you convert compliance issues into dollars and cents of financial gain.

Contact Human Medical Billing to schedule a compliance readiness review or learn more about our end-to-end billing and regulatory support services.
