The biggest flaw with Remote Patient Monitoring (RPM) for years was that if you monitored a patient for 15 days, there were no payments made. To be able to bill CPT Codes 99453 and 99454, it was necessary to collect at least 16 days of data. This has resulted in billions of dollars being lost by providers for post-operative care and acute recovery.
That all changed when the American Medical Association (AMA) announced on December 8, 2025, its new Short-Duration RPM Codes for 2026. The AMA has introduced the ability for healthcare providers to bill for monitoring periods of just 2 to 15 days.
This represents the most significant change in medical coding services in recent history as previously "unbillable" acute data can be converted into actual revenue.
Below are details regarding the update along with the applicable CPT Codes and tips for getting your organization prepared to begin billing these codes starting January 1, 2026.
What Changed for RPM in 2026?:
Change as of Jan. 1, 2026 - RPM can be billed after less than 16 days of use.
The Update: Two new CPT codes will provide reimbursement for 2-15 day period of device supply and monitoring.
The Impact: This changes the way you are able to capture your revenue by eliminating the requirement for sixteen consecutive days of clinical data collection (i.e. weekly BP readings after surgery or during medication adjustment.)
Why the Old 16-Day Rule Was a Problem
Prior to the changes made in 2026, RPM was developed to support chronic disease management. The initial set of codes (99453, 99454), developed by Medicare, were created to report on ongoing, chronic conditions such as diabetes or heart failure.
That model didn’t meet the needs of patients who experience an acute event.
A hypothetical example illustrates this point: A patient has undergone a Total Knee Replacement. For the next seven days, you have provided a connected cuff for the patient to monitor their vital signs to prevent hospital readmission. Although you have completed the necessary work to ensure the patient's safety, under current coding guidelines, since you ended the service at the seventh day, you would be unable to submit a claim for the technical component of RPM services.
Practices had difficult choices to make:
- Monitor without charge.
- Continue to monitor the patient for the full 16 days in order to receive reimbursement (inefficient).
- Not monitor the patient at all.
These two new CPT codes will help providers capture the value of providing episodic care and aligns the payment methodology with clinical realities.
Short Duration RPM Codes (Newly Added Codes):
The AMA and CMS have finalized these additional codes to address this issue and provide a way for providers to capture reimbursement for episodic care.
1. Device Supply for Short Terms (2–15 Days)
This CPT Code captures the cost associated with leasing or renting a RPM device for a short term use.
- What does it cover: Setup and patient education for use of the RPM device.
- Time frame: Must be between a minimum of 2 days and a maximum of 15 days.
- Conditions: Collect RPM device data from at least 2 separate days.
2. Treatment Management for Short Terms
The previous treatment management codes (99457) require 20 minutes of live interaction with a patient. Because of the shorter duration of the RPM services, clinical staff spend less time reviewing data and communicating with the patient.
- What does it cover: Clinical staff time spent reviewing data and communicating with the patient.
- Time Threshold: The new guideline allows for billing for 10 – 19 minutes of clinical staff time in the short window.
Note: The exact RVUs were published in December 11, 2026 CMS Final Rule. Consult your individual fee schedule; however, expect payment rates consistent with the reduced time.
Financial Impact: Finding Hidden Revenue
Few practices are aware of how much “free work” is being done.
If you operate a surgical group, cardiology practice, or an internal medicine clinic, I suspect you have dozens of patients each month that require a couple of days of “watching.”
Let us examine the numbers. If you discharge 50 patients each month that require one week of vital sign tracking:
- Old rules: $0 in revenue.
- New 2026 rules: 50 patients * (supply code + management code).
Regardless of whether we use conservative Medicare reimbursement rates, this quickly converts a cost center into a profit center and provides you with protection against loss. Proper monitoring has been proven to decrease readmission rates, thereby protecting your MIPS scores as well as your value-based care bonus potential.
If you are unclear about calculating this potential, our team at Human Medical Billing would be happy to provide you with a quick review of your unbilled monitoring time to demonstrate the opportunity for growth.
Medical Necessity: When to Use These Codes
You cannot simply replace your previous codes with new ones; you must document the medical necessity behind the claim. CMS and commercial payers will scrutinize these claims to ensure that you are not submitting claims merely for the sake of doing so.
Short-duration RPM is most suitable for the following types of scenarios:
- Post-operative care: monitoring for increases in blood pressure or temperature post-surgery.
- Medication titration: starting a patient on a new beta-blocker and tracking their response over 5 days.
- Acute illness: tracking oxygen saturation while a patient is experiencing a respiratory infection (i.e., COVID-19 or influenza).
- Transitional care: the period from when a patient is discharged from the hospital until the patient's initial visit with their physician.
Not Suitable for:
- Routine visits for patients whose chronic conditions are stable (use the routine 16 day codes for those patients).
- Patients reporting their own data using a non-connected device.
Bonus Update: Virtual Supervision is Now Permanent
While the RPM update may be the most prominent part of the December 11th release, another update also impacts billing for these services in educational environments.
The CMS finalized the rule regarding the ability to utilize live audio/video technologies to satisfy "direct supervision" for Teaching Physicians.
How does this affect billing: Typically, residents or auxiliary personnel monitor the RPM dashboard for alerts. When they find an alert, they flag the issue. However, the supervising physician must then review and take action on the flagged item.
Prior to the update, "direct supervision" required the attending physician to be physically present within the same office suite. With the new rule, the attending physician can review the RPM activity from anywhere and at anytime as long as they have a video/audio feed connection. This will eliminate a significant barrier and allow the billing staff to confidently attach the GC modifier.
Frequently Asked Questions
Billing rules can become very complex. We've provided some commonly asked billing questions by our provider clients currently.
Yes; however, do not duplicate time. For example, if you track time towards an RPM code (e.g., RPM), do not track those same minutes towards CCM for that month. Track each type of time separately.
This is a common scenario. If a patient starts on a short-term plan but complications arise and monitoring continues past 16 days, you should default to the standard RPM codes (99453/99454). Do not bill both short-term and long-term codes for the same period.
Implementation Plan: 5 Steps to Take Now
January 1 is just weeks away. You need to make sure that your systems are ready.
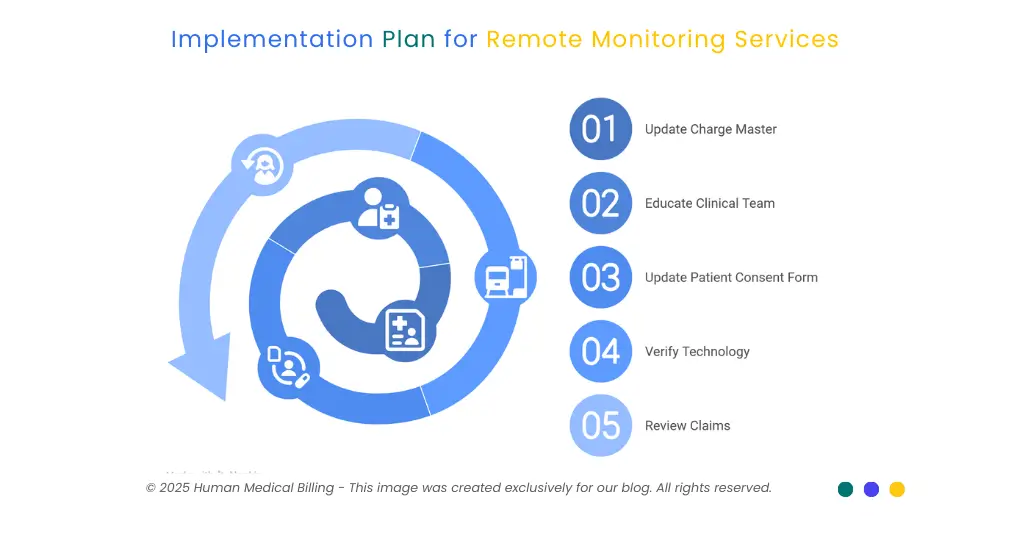
1. Update Your Charge Master
Use those new CPT codes in your EHR system and your billing system. And set the price using 150% of the Medicare allowance, so you're sure to collect maximum reimbursement from all commercial payers.
2. Educate Your Clinical Team
Nursing & Medical Assistants (MAs). They need to understand the difference between acute and chronic use. Document what is the intent of the remote monitoring service. Is this a short term (acute) use, or is this a long term (chronic) use? That documentation will determine which code you select.
3. Update Your Patient Consent Form
Make sure your patient consent form covers “Remote Monitoring Services” broadly enough so that when the patient’s condition changes, and you need to switch to either acute or chronic remote monitoring, you won’t need to get another signed consent.
4. Verify Technology
Are your RPM technology vendors supporting these shorter monitoring windows? Many RPM technology platforms automatically generate billing reports only after 16 days of data. Will you need to adjust your platform to generate a billing report after 2 days of collected data?
5. Review Your First Twenty Claims
In February 2026 review your first twenty claims as soon as possible. Did they pay? Were there requests for records? If you find some of the first twenty claims were rejected, you may need to seek additional assistance.
If your internal staff finds the transition difficult, now would be an excellent time to consider looking into healthcare revenue cycle management services. Healthcare revenue cycle management companies have expert staff that follow these coding updates daily.
How We Can Help
It has been difficult keeping up with the December updates - you want to end the year on a high note and then CMS drops over 500 pages of new rules.
At Human Medical Billing, we serve as your safety net. We do not simply process claims - we identify and capitalize on the opportunities for you. We were aware of this upcoming RPM update and prepared our clients well in advance.
We provide a variety of services to support you including medical credentialing services (enrolling new providers) and medical accounts receivable services (cleaning up an AR mess). We handle the heavy lifting for you.
Here is what we will do for you:
- Verify insurance: Before handing a patient their device we verify whether their plan includes coverage for short-duration RPM.
- Code correctly: Our certified coders understand the difference between a 2-day supply code and a 16-day monitoring code.
- Fight denials: If a payer denies a valid claim, we will appeal it using the new AMA guidelines.
Ready to stop losing revenue on short-term monitoring?
Check out our success stories to see how we helped other practices increase revenue by 15-20% just by fixing coding gaps like this one. You can also read more on our Xpert billing blog for weekly updates.
Final Thoughts
Short-Duration RPM Codes represent a positive development for both providers and patients. This new coding system recognizes that health care does not always occur in months, but rather often takes place in days.
The value of a new code is only realized when it is used. Take the time now to review and modify your workflow accordingly. If you fail to utilize these new codes, you will be essentially working without compensation. However, if you embrace them, they will create a new revenue source that enables you to deliver greater levels of quality patient care.
Do not allow paperwork to impede your ability to create additional revenue streams. Utilize medical billing tools or partner with a trusted third-party provider to assist with the tracking and compliance of the new rules that have been established in your favor. Ensure you are prepared to capture the revenue you have earned.

