What is the 104-Minute Rule for Critical Care Billing?
The 104-Minute Rule refers to a CMS technical correction requiring Medicare patients to receive a full 104 minutes of critical care services before providers can bill both CPT code 99291 and add-on code 99292. This is slightly different from standard CPT guidelines, which allow billing 99292 at just 75 minutes using the midpoint rule.
You can report 99291 for 30-103 minutes of critical care for Medicare billing. When you reach exactly 104 minutes, you can then bill 99291 plus one unit of 99292.
Understanding the Critical Care Time Threshold Confusion
Critical care billing has always been time-based and complex. In 2023, however, CMS dropped a bombshell that many providers still don't fully understand.
In the 2023 Physician Fee Schedule Final Rule, the Centers for Medicare & Medicaid Services issued what they called a "technical correction" that fundamentally changed how Medicare counts time for critical care add-on code 99292.
Here's what happened.
The 2022 PFS final rule said that providers could report 99292 “if 75 or more cumulative total minutes were spent providing critical care.” It fit perfectly with CPT guidelines and what was taught to coders for years.
But CMS backtracked. They said it was an error.
According to the 2023 PFS Final Rule correction, CMS “intended to state that CPT code 99292 could be billed after 104, not 75, or more cumulative total minutes were spent providing critical care.”
This created a major split between the Medicare billing rules and standard CPT coding practices.
CPT Guidelines vs. Medicare Requirements: The Critical Difference
Time-based codes invoke the "midpoint rule" according to the American Medical Association's CPT code book. Under this principle, a unit of time is considered attained when the midpoint has been passed.
For critical care, CPT defines it this way:
- 99291 covers the first 30-74 minutes
- 99292 is added for each additional 30 minutes
- Using the midpoint rule, 99292 can be billed once you pass 15 minutes beyond 74 minutes (which equals 89 minutes total, but commonly applied at 75 minutes)
Medicare does things a little differently.
CMS needs the full 30 minutes beyond the first 74 minutes before you can report 99292. That is 74 + 30 = 104 total minutes.
Here's the breakdown in simple terms:
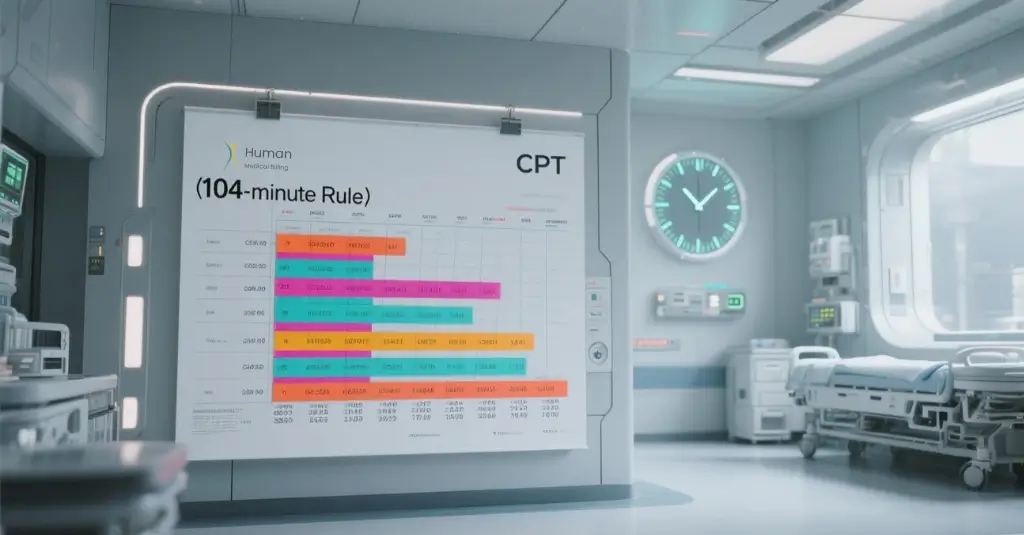
CPT Time Thresholds (Commercial Payers)
- 30-74 minutes: Bill 99291 only
- 75-104 minutes: Bill 99291 + 99292 x1
- 105-134 minutes: Bill 99291 + 99292 x2
Medicare (CMS) Time Thresholds
- 30-103 minutes: Bill 99291 only
- 104-133 minutes: Bill 99291 + 99292 x1
- 134-163 minutes: Bill 99291 + 99292 x2
This gap between 75 and 103 minutes is representative of a significant revenue opportunity being left on the table by many providers.
Why CMS Made This Change (And Why They Say It's Not New)
When providers and professional organizations pushed back, claiming this was a policy change, CMS defended their position.
CMS said that the 104-minute rule has always been its policy. They referred to other parts of the 2022 proposed rule where they correctly stated the threshold of 104 minutes. The error in the final rule, they said, was no more than inconsistent wording, and not a change in policy.
CMS based its stance on the plain language of the CPT code 99292, which describes it as “each additional 30 minutes.” They interpret this literally: you must provide the full 30 minutes, not just reach the midpoint.
The American College of Emergency Physicians, American Medical Association, and other professional societies have documented this discrepancy. While they acknowledge CMS's authority to set Medicare billing rules, the divergence creates real-world headaches for billing departments.
Real-World Impact on Critical Care Revenue
Let's walk through a common scenario to understand the financial impact.
Scenario: An intensivist delivers 85 minutes of critical care to a Medicare patient in respiratory failure.
Under CPT guidelines (commercial insurance):
- Bill 99291 + 99292 x1
- Approximate reimbursement: $350-$400 (varies by region and payer)
Under Medicare CMS rules:
- Bill 99291 only
- Approximate reimbursement: $250-$280
The difference? Approximately $100 to $120 in lost revenue for one encounter.
For a busy ICU or ED seeing dozens of critically ill Medicare patients a month, this adds up to thousands of dollars in under coding.
But the flip side of it is, charging for 99292 prior to reaching 104 minutes for Medicare patients is over coding, which triggers audits and possible compliance issues.
The September 2025 CMS MLN Booklet: Your Official Guide
CMS released a revised Medicare Learning Network MLN Booklet on Evaluation and Management Services in September 2025. This is the most recent, authoritative source for Medicare critical care billing.
The detailed table in the MLN006764 booklet (Table 1: Critical Care Billing) spells out exactly when to bill 99291 and 99292.
Key clarifications from the September 2025 update:
Critical care time with patient is ≥ 104 minutes
- Code to Report: 99291 + 99292
- Key Points: 99292 for each additional 30 minutes beyond initial 74 minutes
Critical care time spent with patient is 30-74 minutes
- Code to Report: 99291
- Key Points: Bill once per date, per patient
Critical care time with patient is < 30 minutes
- Code to Report: Do NOT bill 99291
- Key Points: Does not reach threshold
Also included in the booklet are helpful "If-Then Scenarios" that walk through various billing situations, from single-provider care to split/shared services between physicians and NPPs.
Documentation Requirements Under the 104-Minute Rule
Precise time documentation has never been more important. With payers using AI-based claim review systems and audit rates on the rise in 2025, your documentation needs to be bulletproof.
What Medicare requires:
Total time statement: Record exact minutes, not rounded estimates. Use “Total of 87 minutes of critical care provided," not "approximately 90 minutes.”
Time tracking method: Either exact duration or clock times is acceptable:
- 58 minutes of critical care
- Critical care provided from 14:30 to 15:28 (58 minutes)
Exclusion of separately billable services: If you performed procedures that are not bundled into critical care- such as central line placement or intubation-you must clearly state that this time was excluded.
Example: “Total critical care time: 92 minutes. This excludes 12 minutes for endotracheal intubation, which is billed separately.”
Clinical justification: Your note needs to reflect why the patient needed critical care. Statements such as “patient remains critically ill” will not suffice.
Improved documentation: Patient in acute respiratory failure with SpO2 of 76% on room air who requires immediate high-flow oxygen, ABG analysis, chest X-ray interpretation, and close monitoring for potential intubation. The ventilator settings were adjusted three times based on serial blood gases.
Setting documentation: If providing critical care outside of the ICU, especially in the emergency department, one should clearly document the location of the patient and why the critical care was medically necessary in that setting.
Common Billing Errors to Avoid
Medical billers who handle critical care claims commonly find the following mistakes:
1. Error 1: Applying CPT time rules to Medicare patients
Coders familiar with CPT guidelines might automatically bill 99292 at 75 minutes. For Medicare, this is incorrect and creates compliance risk.
Implement payer-specific edits in your billing system. Flag Medicare claims to apply the 104-minute threshold.
2. Error 2: Rounding up time documentation
Writing "approximately 100 minutes" when the actual time was 94 minutes constitutes fraudulent documentation.
Solution: Train providers to document exact time using either EHR time-tracking tools or by using manual clock time notation.
3. Error 3: Not aggregating non-continuous time correctly
Critical care doesn't have to be continuous. You can combine multiple visits throughout the same calendar day.
Example: Provider sees patient at 08:00 for 45 minutes, returns at 14:30 for 35 minutes, and checks in again at 20:00 for 28 minutes. Total: 108 minutes. Bill 99291 + 99292 x1.
Solution: Create a daily time log for critically ill patients, summing all critical care encounters before coding.
4. Error 4: Same-specialty provider duplicate billing
If multiple physicians from the same group and of the same specialty provide critical care to the same patient on the same day, only one can bill 99291.
Solution: Apply concurrent care rules set by CMS within the same specialty. The first provider bills for 99291; others use 99292 after the combined time reaches 104 minutes.
Split/Shared Critical Care and the 104-Minute Rule
Split or shared visits involve both a physician and an NPP from the same group providing critical care to the same patient on the same day.
For Medicare, the substantive portion rule applies: the provider who performed more than 50% of the total time bills the service using modifier FS.
The 104-minute rule still applies to split/shared critical care.
As CMS clarified in the 2023 PFS Final Rule, Once the cumulative required critical care service time is met to report CPT code 99291, CPT code 99292 could not be reported by a practitioner in the same specialty and group unless and until an additional 30 minutes of critical care services are furnished to the same patient on the same day (74 minutes + 30 minutes = 104 total minutes).
Let's break down an example:
Scenario: Dr. Smith (physician) provides 62 minutes of critical care. Sarah Jones, NP (NPP in same group) provides an additional 48 minutes later that day. Total: 110 minutes.
Correct billing:
- Combined time meets 99291 threshold (30 minutes minimum)
- Combined time exceeds 104 minutes and therefore one unit of 99292 is appropriate
- Sarah Jones provided 48 minutes out of 110 total, or 44%, so Dr.
- Smith performed the substantive portion
- Dr. Smith charges the following: 99291 + 99292 with modifier FS
- Both must document their individual time in the medical record
How This Affects Different Specialties
The 104-minute rule affects various specialties differently:
1. Emergency Medicine:
ED physicians frequently provide critical care but may not have extended time with individual patients before admission or transfer. Knowing this specific 104-minute threshold helps providers avoid both undercoding-where, for example, they would stop their documentation at 75 minutes-and overcoding, whereby they bill 99292 prematurely for Medicare patients.
2. Critical Care Medicine / Intensivists:
ICU physicians often spend well over 104 minutes with critically ill patients. Where the rule most matters is in the 75-103 minute range when commercial payers allow 99292 and Medicare does not.Hospitalists must record time with specificity and payor-specific thresholds when managing ICU patients or providing critical care on medical floors.
3. Anesthesiology:
Anesthesiologists providing critical care services, separate from anesthesia for procedures, are subject to the same time rules and documentation standards.
Technology Solutions for Time Tracking
In response to increased scrutiny over documentation, EHR vendors have developed new time-tracking tools designed especially for critical care.
These systems generally offer:
- Automated time capture: Click "start critical care" and "stop critical care" buttons that automatically log duration
- Exclusion tracking: separate timers for bundled vs. separately billable procedures
- Daily aggregation: automatic summation of non-continuous critical care episodes throughout the day
- Payer-specific alerts: Warnings when approaching billing thresholds for 30 minutes, 104 minutes, and 134 minutes
- Documentation templates: the pre-built note templates that prompt for the required elements
Technology is helpful, but the provider is still responsible for correct time reporting. Automated systems should augment documentation, not replace clinical judgment about what constitutes critical care time.
Revenue Cycle Management Implications
For healthcare revenue cycle management services teams, the 104-minute rule creates both challenges and opportunities.
Challenges:
- The billing teams have to implement payer-specific logic within their coding workflows. Medicare claims require different time calculations than that of commercial insurance claims for the exact same service.
- Training staff on the nuance between CPT and CMS rules takes time and resources.
- Auditing is becoming more complicated when reviewing mixed-payer critical care claims
Opportunities:
- Providers who had previously stopped documenting at 75 minutes, thinking they'd captured maximum reimbursement, may be leaving money on the table. If they provide 85-95 minutes of care but only document 75, they are losing legitimate revenue under both systems.
- Proper education can help physicians document to the actual time spent, thus increasing the appropriate billing for extended critical care.
- Clean claim rates improve when the billing teams catch payer-specific errors before submission. Organizations providing medical billing services have found that comprehensive critical care billing audits usually detect 3-7% revenue recovery opportunities.
Denial Management Strategies
Critical care claims have higher rates of denial compared to many other E/M services, particularly when billed from emergency departments.
Common denial reasons relating to the 104-minute rule:
- Time threshold not met - Payer audit shows documentation does not support 104 minutes for Medicare
- "Services not separately identifiable"- Documentation does not clearly exclude bundled services from critical care time
- "Insufficient medical necessity" - Clinical narrative does not justify critical care level of service in appealing these denials.
- Gather complete documentation: The medical record should reflect the time, clinical judgment, and interventions performed.
- Cite payer-specific policy: Reference September 2025 CMS MLN Booklet and specific policy guidance
- Provide time logs: If time was non-continuous, submit a detailed timeline showing each critical care encounter
- Emphasize clinical complexity: exemplify high-level medical decision-making, organ system failure, and risk of life-threatening deterioration.
Organizations providing strong denial management services report that critical care appeals are successful 40-60% of the time, as long as proper documentation exists.
Best Practices for Compliance
A systematic approach is paramount to remain compliant while maximizing appropriate reimbursement.
- Provider education: Provide quarterly training regarding critical care documentation requirements. Specialty-specific scenarios should be included along with real examples from your organization.
- Pre-bill audits: A certain percentage of critical care claims are reviewed prior to their submission. Potential issues are flagged for provider clarification.
- Payer policy monitoring: CMS issues and revises policies regularly.
- Internal Audits: Perform retrospective reviews of paid critical care claims. Look for patterns of undercoding, overcoding, or documentation deficiencies.
- EHR optimization: Collaborate with your EHR vendor to develop critical care-specific templates and time-tracking tools that ensure templates prompt for all required elements of documentation.
- Collaborative approach: Physicians should be included, along with coders, compliance staff, and revenue cycle teams in this process. Develop a common understanding of what is needed for documentation and revenue implication.
Working with Professional Medical Billing Partners
Most healthcare organizations find that critical care billing complexity is best met with specialized expertise.
When assessing medical billing services or considering the outsourcing of revenue cycle functions, look for partners with:
- Specialty-specific experience: Critical care billing is quite different from primary care or surgical billing. Ask about their experience with codes 99291/99292.
- Payer expertise: Partners should know the rules of both Medicare and commercial payers, including nuances around the 104-minute rule.
- Technology capabilities: Modern medical A/R services employ the latest software with the ability to apply payer-specific edits automatically.
- Denial management track record: Request data regarding the critical care claim denial rates and appeal success rates.
- Credentialing support: Medical credentialing services ensure that providers are properly enrolled with all payers in order to avoid unnecessary denials.
- Educational resources: The best partners don't just submit claims; they educate your clinical team on best practices in documentation.
In-house billing or with the help of a medical billing service, there can be no compromise on the 104-minute rule for financial health.
Looking Ahead: Regulatory Trends
The controversy over the 104-minute rule reflects continuing tension between CMS and the broader medical community about time-based billing. Professional societies continue to advocate that the regulations for CPT and Medicare be harmonized.
CHEST supported this request with CMS for policy change, noting it "devalues the first hour by 30%." The 104-minute rule remains in effect for the foreseeable future. This means that providers should document and code accordingly.
Watch for:
- Future PFS final rules: While CMS may reconsider their stance in a future rulemaking, they have defended the threshold of 104 minutes on several occasions.
- MAC guidance updates: Medicare Administrative Contractors periodically release clarifying guidance regarding critical care billing. Check your MAC website for updates
- Changes to commercial payers policies: Some commercial payers will follow CMS rules, and some still keep standard CPT timing. Check each payer's rules individually.
- Audit Trends: With the growth in Medicare Advantage enrollment and an expansion of CMS RADV audits, critical care claims will face heightened scrutiny.
Frequently Asked Questions
No. Most commercial payers follow the standard CPT guidelines which allow billing 99292 at 75 minutes. Always check specific payer policies.
No, for Medicare patients, you must reach exactly 104 minutes before billing 99292. If you are at 103 minutes, bill only 99291.
Only bill 99291. You are in the 30-103 minute range, which does not meet the threshold of 104 minutes to add 99292.
Document each critical care service date separately noting the start/stop times or duration. Sum the total time for the calendar day. Make sure each encounter meets the definition of critical care, not a routine follow-up visit.
No. The 104-minute rule only applies to time-based codes 99291 and 99292. Codes for pediatric and neonatal critical care, 99468-99472, 99475-99476, are per-day codes and are subject to different billing rules.
Key Takeaways
The 104-Minute Rule represents a critical divergence between CPT coding guidelines and Medicare billing policy. Whereas the CPT guidelines allow 99292 at 75 minutes, Medicare requires the full 104 minutes before providers can bill both 99291 and 99292.
For billing professionals and providers:
- Implement payer-specific coding edits in your billing system
- Document the exact time with precision, do not round or estimate
- Aggregate non-continuous critical care encounters throughout the calendar day
- Clearly exclude separately billable procedures from critical care time
- Understand the substantive portion rule for split/shared visits
- Stay current with CMS MLN updates and MAC guidance
- Consider specialty healthcare revenue cycle management services if you have complex billing situations.
The financial stakes are real: undercoding costs revenue, and overcoding creates compliance risk. Getting it right requires knowledge, attention to detail, and ongoing education.
Expert Help for Critical Care Billing
Critical care billing doesn't need to be overwhelming. Here at Human Medical Billing, we're experts in helping healthcare providers manage complex billing scenarios like the 104-minute rule.
Our comprehensive healthcare revenue cycle management services include:
- Payer-specific coding expertise for both Medicare and commercial plans
- Advanced medical coding services with certified critical care specialists
- Proactive denial management services to appeal rejected claims
- Complete medical accounts receivable services to accelerate payment collection
AI technology in medical billing that applies payer-specific rules automatically Whether you are an intensivist, emergency physician, hospitalist, or run a multispecialty group, we understand the unique challenges of critical care billing. Ready to optimize your critical care revenue?
You can learn more about how our services work by reading our success stories from healthcare providers who have partnered with us. Browse our Xpert billing blog for more insights on best practices in medical billing, or review our comprehensive FAQs section.
Have questions about your current billing processes?
Please feel free to contact us today for a free consultation. Learn more about us and how Human Medical Billing can help you maximize reimbursement while maintaining compliance.