Adaptive Payer Management
Our billing specialists stay on top of evolving insurer rules for chiropractic care, from Medicare adjustments to private plan updates. By monitoring policy shifts and payor trends, we help clinics minimize payment disruptions and keep revenue cycles strong.
Live Monitoring for Rule Updates
Our team actively tracks regulatory changes affecting chiropractic billing, including CPT code updates and Medicare’s annual requirements. Every claim is checked against current payer standards, ensuring accurate coding and supporting documentation. This vigilance helps keep your practice audit-ready and compliant while protecting timely reimbursement.
Expert Reviews Recover Lost Revenue
Our team pinpoints denial causes specific to chiropractic—such as bundled services or payer restrictions—by auditing records and verifying documentation. We correct omitted codes, clarify therapy necessity, and pursue appeal processes. Persistent follow-up and targeted resubmissions help you reclaim revenue and build a more reliable payment pipeline.
Dedicated Chiropractic Billing Specialists
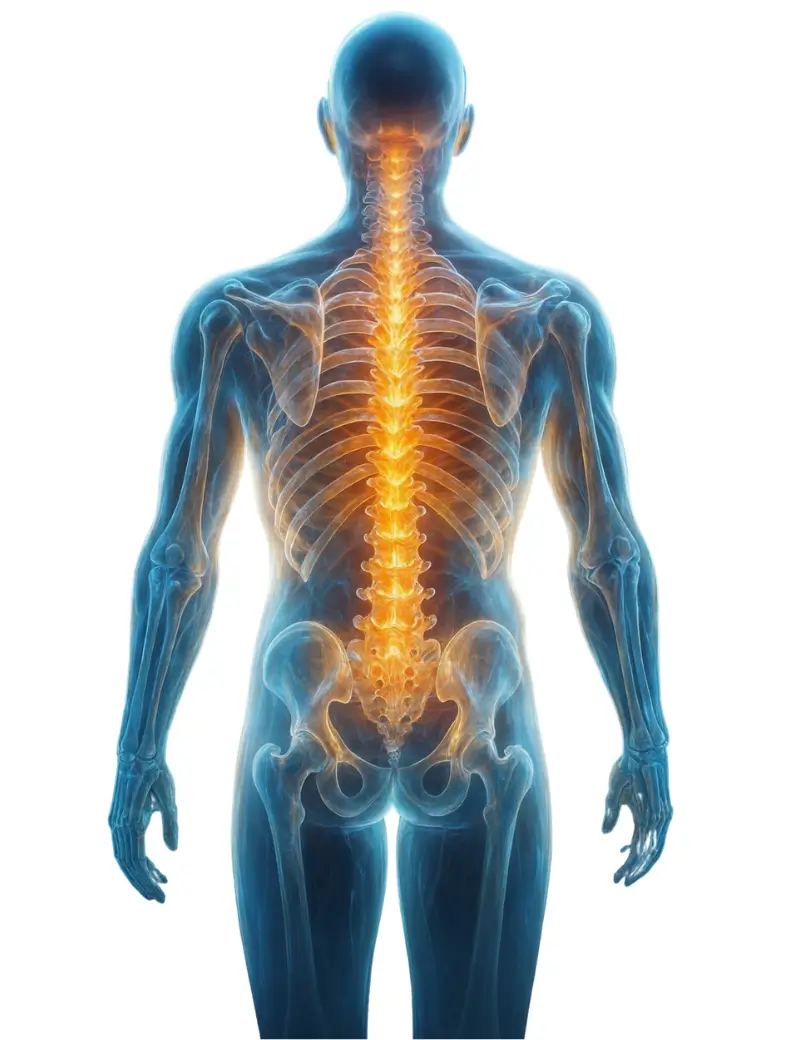
Every claim is managed by experts experienced in chiropractic-specific billing for modalities, therapies, and insurance types. Our team knows the latest payer rules, modifier requirements, and compliance standards for spinal care. By focusing only on chiropractic practices, we optimize each submission for accuracy, minimizing errors and accelerating reimbursements across Medicare and commercial payers.